CCJ Patient Experience Survey
Read about the survey's goals and instructions to complete this survey.
Read about Spine and Brain Advocate's Mission and About
Read about how Spine and Brain plans to Champion Changes to Healthcare
Read the latest Summary Report on the CCJ Patient Experience
Review the compiled summary of 2nd Radiology Report Outcomes and Get 2nd Opinion Radiology Reports by CCI expert Radiologists

/78
I am willingly providing my personal and health information and provide my express consent for Spine and Brain Advocate to use my information for statistical reporting and lobbying purposes. I am aware my personal information (address, name etc.) will not be disclosed without consent. I understand that at any time I do not wish Spine and Brain Advocate to use my data, I can request in writing that my information be removed from the database.

YES
NO
/78
What is your First Name?
/78
What is your Last Name?
/78
Enter your Birth Month and Year in this format: 04/1998
/78
What was your biological gender at birth?
Female
Male
Prefer not to say
/78
How many years since your illness began until today?

0 - < 1 year
1 - 3 years
4 - 7 years
8 - 10 years
More than 10 years
/78
Describe your illness onset history. Select the one that you believe is the main root cause.

Head/Neck Injury (Motor Vehicle Accident, Sports and Recreation, Trip or Fall etc.)
Dental Appointment
Chiropractic Appointment
Viral Infection
Tick Bite or Bacterial Infection
Elhers-Danlos Syndrome / Hypermobility Disorder
Chiari Malformation
Surgery in the head or neck area or requiring intubation
Tumor
Congenital Condition not mentioned above
Rheumatoid Arthritis
Mast Cell Activation Syndrome or Prolonged allergic reaction
Chronic Black Mold
Covid (any variant)
None of the above
/78
If you indicated a physical trauma / accident triggered onset of illness, what was your accident? e.g. horse, motor vehicle, skiing etc. If you did not select this, write N/A
/78
What was your initial / 1st diagnosis after illness onset? Select 1 - 2 that you believe are the most relevant.

ME/CFS
Fibromyalgia
Psychosomatic / Depression / PTSD
Whiplash / Whiplash Associated Disorder
Spinal Stenosis
Chiari Malformation
Eagles Syndrome
Thyroid Gland Disorders / Cancer
Spina Bifida
Lyme Disease
Tramatic Brain Injury / Concussion / Post-Concussive Syndrome
Anklosing Spondylitis
Arthritis (Rheumatoid/Osteoarthritis)
Brain Herniation
Cerebrospinal Fluid Leak
Tarlov / Perineural Cyst / Spinal Meningeal
Stenosis (cervical, vascular, foraminal etc.)
Degenerative Disc Disease
Ehlers Danlos Syndrome (EDS) / Connective Tissue Disorders
Facet Joint Syndrome
Hydrocephalus
Kyphosis
Mast Cell Disorders / Mastocytosis
Scoliosis
Spinal Instability
Tethered Cord Syndrome
Vertigo
Vertebrobasilar Artery Syndrome
Intracranial hyper/hypotension
Thoracic Outlet Syndrome
Mold Allergy
Tinnitus
Pituitary Disorders
Post-Viral Syndrome
Grisel Syndrome
"too much stress"
Metabolic Disorder
Hernia
None of the above
/78
Approximately how much time did it take to receive your first diagnosis?

0 - < 1 year
1 - 3 years
4 - 7 years
8 - 10 years
more than 10 years
/78
What is your Current Level of Disability? Select one that best describes your current situation.

0 Normal Function
3 Mobile without assistance but signs and symptoms
5 Impaired daily activities
7 Restricted to Home
10 Bedridden, need caregiver, difficult to eat or talk
/78
What was your Level of Disability at Illness Onset? Select one that best describes your situation.
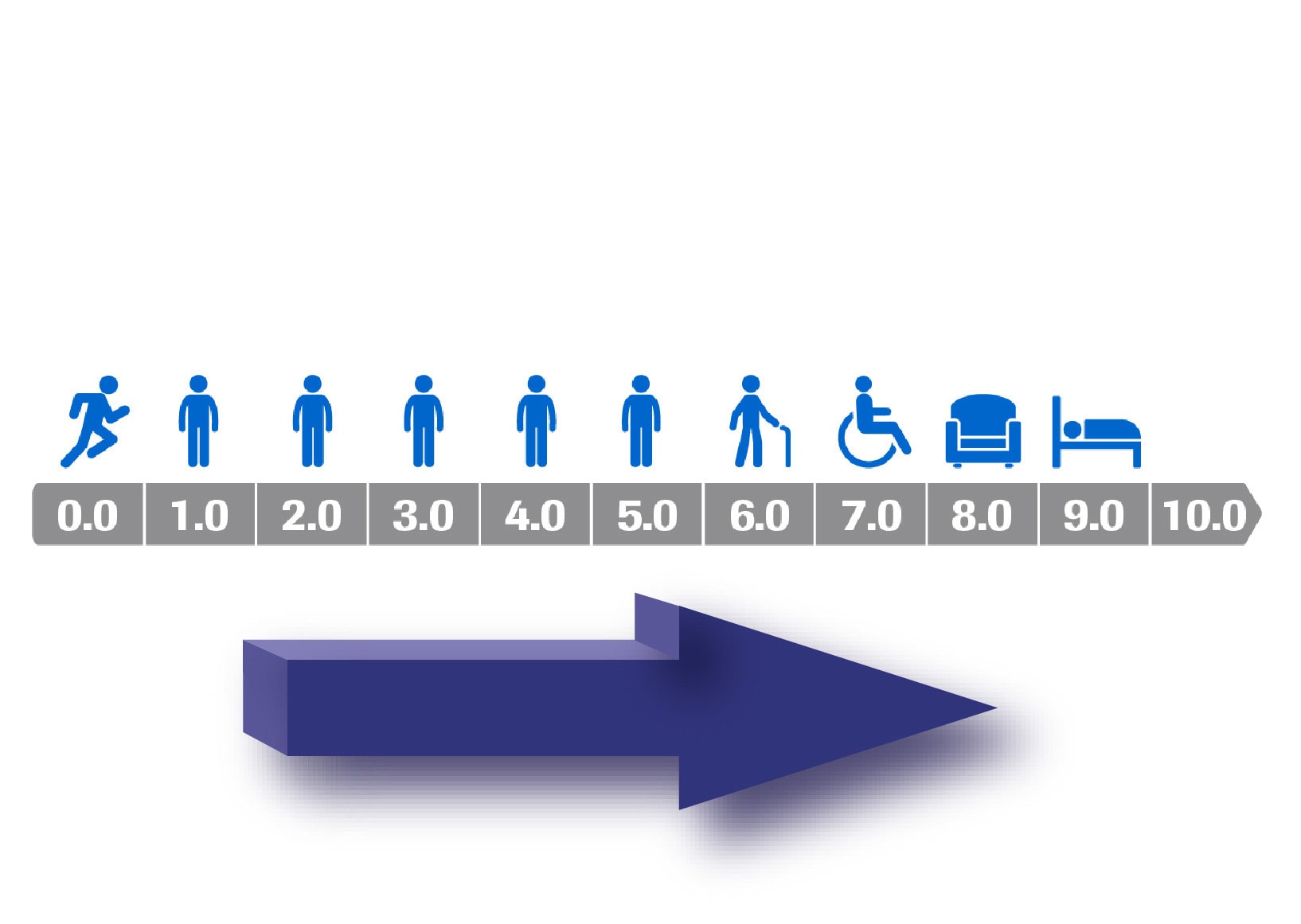
0 Normal Function
3 Mobile without assistance but signs and symptoms
5 Impaired daily activities
7 Restricted to Home
10 Bedridden, need caregiver, difficult to eat or talk
/78
What are the worst signs and symptoms have you experienced from time of illness onset to now? Select your top 5 worst symptoms.
Exhaustion / Fatigue that is not relieved by sleep or rest and resulting in substantial reductions in previous levels of daily activites
Pain that is often widespread. Includes myofascial pain, joint pain, abdominal pain or migranes, headaches etc.
Headaches or pressure in the head
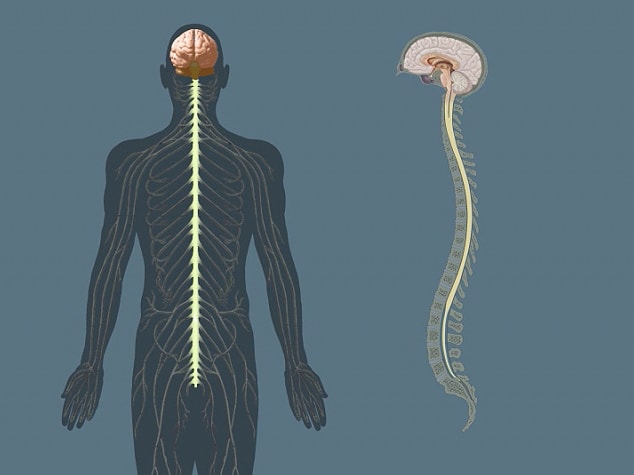
Neurological manifestations such as issues with vision or hearing, sensitivity to light or noise, muscle weakness, muscle twitching, tingling and numbness etc.
Cognitive manifestations such as impaired memory, difficulty with paying attention, finding words, comprehending information, slowness of thought etc.
Post-exertional fatigue with rapid physical or mental stamina and recovery is slow, often 2 to 24 hours or longer
Sleep disturbance including unrefreshing sleep, nonrestorative sleep or disturbance of sleep quality
Autonomic manifestations including (POTS) postural orthostatic Trachyardia, dizziness, fainting, loss of balance, nausea, bladder dysfunction, Mast Cell Activation Syndrome
Troubles swallowing / choking on food
Neck pain and symptoms increase with neck movement
Limited neck mobility / neck muscle stiffness
I often or always feel an "internal tremor" that is not visible to the eye
Respiratory Issues such as shortness or trying to catch breath, or involuntarily stop breathing
Loss of feeling/sensation in all four limbs
Hand(s) sometimes or always a bluish color and/or I have arm pain, numbness and swelling
Ringing or buzzing in the ears (tinnitus)
Migraines
Chronic Migraines (at least 15 days per month)
Fainting or passing out
Occipital Neuralgia - headaches that feel like severe piercing, throbbing or shock-like pain in the upper neck, back of head or behind the ears
Spinal cracking, grinding or popping sounds
Pain in the tailbone area
Partial or complete paralysis
Leg/Arm weakness or loss of strength
Hand Grip Weakness / Dropping things
Partial or complete loss of sensation/feeling in hands or feet
Seizures
Difficulty reading and writing
Decreased alertness
Partial or complete inability to be upright
Lethargy or changes in level of consciousness
Dystonia / Involuntary muscle contractions / shaking episodes
Loss of balance / Dizziness / Lightheaded
Vertigo / room spinning
Nausea / Vomiting
Sound sensitivity / Ringing in the Ears
Light sensitivity / Eye Pain / Blurred Vision / Double Vision
Depression
Anxious / Fight, Flight or Freeze
Gait / Walking Issues
Bowel or Bladder problems holding/controlling
Difficulty Speaking
Facial Weakness / Numbness
Back pain
Neck pain
Racing heartrate without physical exertion
Pain in the ribs / costochondritis
Flushing of the face / neck / chest
Hand Tremors
Constipation
Blood in stool
Trouble Urinating
Nighttime Urination that interrupts your sleep
Painful Urination
Arm numbness or tingling
Leg numbness or tingling
Joint Pain
Dizziness or lightheaded or feeling faint when standing up from sitting or lying down
Dizziness or lightheaded or feeling faint when turning head left or right
Dizziness or lightheaded or feeling faint when looking up or down
Dizziness or lightheaded or feeling faint after exposed to heat e.g. hot bath, day or shower
Difficulty concentrating
Difficulty understanding when people are speaking to me
Cannot find / forgetting words
Poor memory of what happened yesterday or two days ago
Loss of consciousness / blacking out
Memory Loss
Vision Flashes / Auras
Poor coordination
Increased pain / fatigue / flares after turning head or looking up and down
Slurred Speech
Neck pain when driving / riding on bumpy roads
Muscle Pain at rest
Cramps or stiffness in muscles
Pain when lying down
Pain when walking up stairs/incline
I have tailbone pain / sacral pain
Lymph Nodes Swollen / Disorders
Frequent Infections
Feeling heartbeats / palpitations
Pain to touch neck and/or head
Sharp electric shock type pains in the head, neck or arms
Hear clicking, sliding, popping or grinding in the back of head or neck
Jaw Pain / TMJ
Facial numbness i.e. numbness in the lip(s), chin, cheeks etc.
Hearing heartbeat in ears
Stiffness and pain in the spine / have trouble moving around
Pain and swelling in your joints such as your fingers, knee or elbow
Sharp pains when turning your head side to side
Floaters (dark shapes that float across your vision)
Unable to sleep on back due to pain in back of head/upper neck
Can only sleep on back due to symptoms
Painful to sleep on side
Can only sleep on one side due to symptoms
Can only sleep on incline like a reclining chair or couch due to symptoms
Pain/symptom relief with wearing a cervical collar (hard or soft)
Can hear and/or feel your upper spine moving when changing to certain positions
/78
How satisfied are your with your FAMILY DOCTOR's investigation of Craniocervical (head and neck) Disorders?

Extremely dissatisfied
Very dissatisfied
Somewhat dissatisfied
Neutral
Somewhat satisfied
Very satisfied
Extremely satisfied
I do not have a family doctor
/78
How satisfied are your with your local SPECIALIST(S)' investigation of Craniocervical (head and neck) Disorders?
Extremely dissatisfied
Very dissatisfied
Somewhat dissatisfied
Neutral
Somewhat satisfied
Very satisfied
Extremely satisfied
I do not have a specialist
/78
How satisfied are your with the local RADIOLOGIST(S)' investigation of Craniocervical (head and neck) Disorders?

Extremely dissatisfied
Very dissatisfied
Somewhat dissatisfied
Neutral
Somewhat satisfied
Very satisfied
Extremely satisfied
I have not had any imaging of my head and/or neck
/78
"Medical gaslighting" is when a healthcare professional downplays or blows off a patient's symptoms and might even say his/her issues are imaginary or in one's head or exaggerated. Since illness onset, how many times have you been medically gaslight?

0 times
1-3 times
4-7 times
8-11 times
12 times or more
/78
How many times have you gone to the emergency department for your illness?

0 times
1-3 times
4-7 times
8-11 times
12 times or more
/78
How did you approach investigating Craniocervical Disorder(s)? Select the two that most describe your experience.

My local doctor/specialist referred me to investigative testing for Craniocervical Disorders
Members of a patient support/advocacy group referred me to doctors that investigative testing for Craniocervical Disorders
I search on the web and found doctors to investigate Craniocervical Disorders
It would describe the process as "trial and error" in trying to find the right doctors to investigate Craniocervical Disorders
I used only one (1) remote doctor to investigate Craniocervical Disorders
I used 2 to 3 remote doctors to investigate Craniocervical Disorders
I used 3 to 5 remote doctors to investigate Craniocervical Disorders
I used 6 or more remote doctors to investigate Craniocervical Disorders
/78
Once it was decided to investigate craniocervical junction for disorders, how many years did it take to complete the CCJ investigation (meaning, investigate craniocervical junction structure, blood & CSF flow) from start to finish?

0 - < 1 year
1 - 3 years
4-7 years
8-10 years
More than 10 years
I have not had Craniocervical Disorders ruled out because my doctor(s) will not investigate.
I am in process of investigating Craniocervical Disorders with my doctors support
I am in process of investigating Craniocervical Disorders on my own because my doctors are not supporting me
/78
Approximately how many years from illness onset, did it take to receive your first Craniocervical Disorder Diagnosis?

0 - < 1 year
1 - 3 years
4 - 7 years
8 - 10 years
More than 10 years
An investigation has not been completed and therefore I do not have a craniocervical disorder diagnosis.
/78
How many doctors did it take to get a Craniocervical Disorder(s) Diagnosis?

This question does not apply because I am in process of investigating Craniocervical Disorders or I have not started any investigations
1-3 healthcare professionals assisted in my Craniocervical Disorder Diagnosis
4-7 healthcare professionals assisted in my Craniocervical Disorder Diagnosis
8 or more healthcare professionals assisted in my Craniocervical Disorder Diagnosis
/78
What is your clivo-axial angle (CXA) measurement in neutral position? (i.e. skull base angle/brainstem deformity) NOTE: If you have more than one CXA measurement, provide your most abnormal measurement.
Normal - CXA Neutral 150 to 170 degrees
Borderline Abnormal - CXA Neutral 136 to 149 degrees
Abnormal / Pathological - CXA Neutral ≤ 135 degrees (CXA kyphosis)
Received "normal brainstem" diagnosis but no CXA in neutral position measurement
Received "abnormal/brainstem deformity" diagnosis but no CXA in neutral position measurement
I have not received Head & Neck imaging
I received head and neck imaging but no CXA measurement in neutral
/78
What is your clivo-axial angle (CXA) measurement in flexion position? (i.e. skull base angle/brainstem deformity) NOTE: If you have more than one CXA flexion measurement, provide your most abnormal measurement. Important Note: The research in this area is in its absolute infancy and by no means can be regarded as good science.
Normal - CXA Flexion ≥ 140 degrees
Borderline Abnormal - CXA Flexion 135 to 139 degrees
Abnormal / Pathological - CXA Flexion ≤ 134 degrees
As of today, I have not received Head & Neck imaging
I received head and neck imaging but no CXA measurement in flexion
/78
What is your clivo-axial angle (CXA) measurement in extension position? (i.e. skull base angle/brainstem deformity) NOTE: If you have more than one CXA measurement provide your most abnormal measurement. Important Note: The research in this area is in its absolute infancy and by no means can be regarded as good science.
Normal - CXA Extension ≥ 160 degrees
Abnormal - CXA Extension ≤ 159 degrees
I have not received Head & Neck imaging
I have received Head & Neck imaging but no CXA in extension measurement
/78
What is your Grabb-Oakes measurement? (i.e. ventral brainstem compression) NOTE: If you have more than one measurement (e.g. flexion, extension) provide your most abnormal measurement.

Normal < 6 mm
Borderline Abnormal ≥ 6 mm and < 9 mm
Abnormal / Pathological ≥ 9 mm
Received "normal" diagnosis but no Grabb-Oakes measurement
Received "abnormal" brainstem compression diagnosis but no Grabb-Oakes measurement
I have not received Head and Neck imaging
I received head and neck imaging but no Grabb-Oakes measurement
/78
What is your Basion-DENS Interval (BDI) measurement in neutral position? (i.e. cranial settling) If you have more than one measurement, provide your most abnormal measurement.

Normal < 10 mm
Abnormal ≥ 10mm
Received "normal" diagnosis but no BDI neutral measurement
Received "abnormal" / "Cranial Settling" diagnosis but no BDI neutral measurement
I have not received head and neck imaging
I received head and neck imaging but no BDI neutral measurement
/78
What is your Basion-DENS Interval (BDI) measurement in flexion position? (i.e. cranial settling) If you have more than one measurement, provide your most abnormal measurement. Note: The research in this area is in its absolute infancy and by no means can be regarded as good science.
Normal < 12 mm
Abnormal ≥ 12 mm
Received "normal" diagnosis but no BDI in flexion measurement
Received "abnormal" / "Cranial Settling" diagnosis but no BDI in flexion measurement
I have not received head and neck imaging
I received head and neck imaging but no BDI measurement in neutral
/78
What is your Basion-DENS Interval (BDI) measurement in extension position? (i.e. cranial settling) If you have more than one measurement, provide your most abnormal measurement. Note: The research in this area is in its absolute infancy and by no means can be regarded as good science.
Normal < 10 mm
Abnormal ≥ 10mm
Received "normal" diagnosis but no BDI in extension measurement
Received "abnormal" / "Cranial Settling" diagnosis but no BDI in extension measurement
I have not received head and neck imaging
I received head and neck imaging but no BDI extension measurement
/78
What is your Basion-AXIAL Interval (BAI) measurement? (i.e. Atlanto-occipital/C0-C1 dissocation injury) NOTE: If you have more than one measurement (e.g. flexion, extension) provide your most abnormal measurement.
Normal < 12 mm
Abnormal ≥ 12 mm
Received "normal" diagnosis but no BAI measurement
Received "abnormal" / "Craniocervical Instability / Atlanto-occipital dissociation" diagnosis but no BAI measurement
As of today, I have not received head and neck imaging
I received head and neck imaging but no BAI measurement
/78
What is your Translational BAI (T-BAI) measurement? (i.e. horizontal instability / skull sliding over spine in flexion and extension positions)

Normal < 1 mm
Borderline Abnormal ≥ 1 mm and ≤ 2 mm
Abnormal / Pathological > 2 mm
Highly Abnormal >4 mm
Received "normal" radiological findings but no T-BAI measurement provided
Received "abnormal" horizontal instability diagnosis but no T-BAI measurement provided
As of today, I have not received Head and Neck imaging
I received head and neck imaging but no T-BAI measurement
/78
What is your Sum (i.e. left & right) C1 Lateral Mass Overhang on C2 measurement (i.e. lateral bending; ear to shoulder measurement)?

Normal ≤ 7 mm (adult) (total / sum for both sides)
Abnormal / Pathological ≥ 7 mm (adult) (total / sum for both sides)
Highly Abnormal ≥ 10 mm (adult) (total / sum for both sides)
Received "normal" radiological findings but no Lateral Mass Overhang measurement
Received "abnormal" cervical instability diagnosis but no Lateral Mass Overhang measurement
As of today, I have not received Head and Neck imaging
I received head and neck imaging but no Lateral Mass Overhang measurement
/78
What is your Power's Ratio measurement? (i.e. head has moved forward on the upper neck)

Normal < 1 mm
Abnormal > 1 mm
Received "normal" diagnosis but no Power's Ratio measurement
Received "abnormal" craniocervical instability diagnosis but no Power's Ratio measurement
As of today, I have not received Head and Neck imaging
I received head and neck imaging but no Power's Radio measurement
/78
What was the result of your traction test (i.e. manual with a device or collar; halo or invasive)? Select the answer that best describes your results.

During traction, complete relief of symptoms
During traction, greatly relieved of symptoms
During traction, somewhat relieved of symptoms
During traction, minor relief of symptoms
During traction, no relief of symptoms
During traction, my symptoms worsened
I have not tried a traction test
/78
List of Doctors that conducted investigation(s) for Craniocervical Disorders. Select all that apply.

My Family Doctor
My Rheumatologist
My Neurologist
My Neurosurgeon
My Physiotherapist
My Chiropractor but not NUCCA or Atlas Orthogonal Certified
My NUCCA or Atlas Orthogonal Certified Chiropractor
My Osteopath
My Orthopedic Surgeon
My Sports Medicine Doctor (M.D.)
My Physiatrist
My Regenerative Medicine Doctor
My Internal Medicine Doctor
I had to go out of State/Province to get my craniocervical junction investigated
I had to go out of Country to get my craniocervical junction investigated
I had my craniocervical junction investigated locally in my City or nearby
Another way not listed above
/78
Names of the Doctor(s) that gave you a Craniocervical Junction Disorder Diagnosis (CCI, AAI, Cervico Medullary Syndrome). Select all that apply.

Dr. Paolo Bolognese in Hyde Park, New York, USA
Dr. Fraser Henderson in Silver Spring, Maryland, USA
Dr. Sunil Patel in Charleston SC, USA
Dr. Henry Ahn in Toronto, Canada
Dr. Gilete in Barcelona, Spain
Dr. Sasha Blaskovich in Langley, British Colombia
Dr. Evan Katz in Boulder, Colorado
Dr. Ross Hauser in Fort Myers, Florida
Dr. John Pitts in Broomfield, Colorado
Dr. John Schultz in Broomfield, Colorado
Dr. Chris Centeno, Broomfield, Colorado
Dr. Michael Fehlings, Toronto, Canada
Dr. Gordon Ko, Toronto, Canada
Other - add the doctor's name, City and Country
Other
/78
On average, how much money do you spend per year to "conservatively manage" your illness? (i.e. medications, physiotherapy, pain management, aids, medical appointments etc.)

Although I need to conservatively manage my illness, I cannot afford to because of my income
$0 to $999. per year to conservatively manage my symptoms
$1000 to $2999. per year to conservatively manage my symptoms
$3000 to $4999. per year to conservatively manage my symptoms
$5000 to $9999. per year to conservatively manage my symptoms
More than $10,000 per year to conservatively manage my symptoms
/78
At any point in your life, which diagnosis have you OFFICIALLY received? Select all that apply to you.

Chiari Malformation
Eagles Syndrome
Craniocervical Instability / Atlantooccipital Dissociation (C0-C1)
Atlantoaxial Instability (C1-C2)
Cervical Stenosis
MCAS Mast Cell Activation Syndrome
EDS Ehlers-Danlos Syndrome or Hypermobility Disorder
Intracranial HYPERtension
Loss of Cervical Lordosis
Loss of Lumbar Lordosis
Tethered Cord Syndrome
Thickened Filum
Subaxial Cervical Instability
Tarlov Cyst
Intracranial HYPOtension
POTS Postural Orthostatic Trachyrdia Syndrome
Jugular Vein Stenosis
Pituitary Gland Abnormality
Basilar Invagination
Thoracic Outlet Syndrome
Lyme Disease
Chronic Viral Infection
Whiplash / Chronic Whiplash
Vascular Stenosis or Compression
Herniated Discs
Budging Discs
Facet Osteoarthritis
Cerebral Spinal Fluid CSF Leak
Cervical Tubercle Bone
Forminal Stenosis
Cervical Kyphosis
Brainstem Kyphosis or Kinking
Rheumatoid Arthritis
Hypothyroidism
Hyperthyroidism
Syringomyelia
Spinal Osteoarthritis
Spinal Cord Injury (SCI)
Spondylosis / Degenerative condition causing vertebral body to slip forwards
Retrolisthesis / Degenerative condition causing vertabral body to slip backwards
Osteoporosis
Congenital Spine Condition
Congenital Brain Condition
Spinal Bifida
Other - please add
Other
/78
What investigation tool(s) or technique(s) were successful in helping to identifying a brain or spine condition? Select all that apply.

X-Ray Lateral
X-Ray Davis Series or a Flexion and Extension XRay
Supine MRI
Upright MRI
Open MRI
Digital Motion XRay (DMX)
Physical Assessment
CT Scan
Rotational CT Scan
CT Flexion and Extension or Rotational
Supine MRI with Flexion and Extension
Upper Cervical MRI with Head Coil
I have not had any Head or Neck Imaging
None of these tools or techniques helped with my craniocervical diagnosis
CT Venogram
MRI of the brain and spine with contrast
speculative lumbar epidural blood patch
CT Myelogram
MRI Myelogram
EKG
MRI Brain and Cervical Spine without contrast with CSF Flow Study
MR Angiogram
CT Angiogram
Non-invasive Cervical Traction (manual, device or collar)
Invasive Cervical Traction conducted by a surgeon
Other
Other
/78
What do you believe is the TOP thing that can be done to improve a Craniocervical Disorder diagnosis?

Family doctors can order most appropriate testing that a CCI surgeon would order.
Radiology technicians can make sure they produce quality images e.g. by using head coils etc.
Better imaging technology can be more accessible. e.g. 3T, DMX, upright MRI
Radiologists required to do standard craniocervical junction measurements ADI, CXA etc.
Neurologists trained in craniocervical junction disorders.
Neurosurgeons, Spine Surgeons, Orthopedic Surgeons can be trained on dynamic craniocervical junction disorders.
Researchers debunk the full spectrum of craniocervical junction disorders (not just severe/obvious/cases of fracture but also less obvious/dynamic cases) and link head/neck trauma and bacterial/viral infections to craniocervical junction disorders.
Craniocervical junction specialists - both surgeons and regenerative medicine, collaborate to raise the bar on diagnosis and treatment of craniocervical junction disorders.
Medical Schools must add the full spectrum of Craniocervical Junction Disorders to their curriculum
/78
What types of treatments have you undergone for your brain and/or spine conditions? Select all that apply.

Spinal Fusion in my country
Spinal Fusion outside my country
Decompression Surgery
Blood Patch
Mesenchymal Stem Cell Injections in Spine
PRP Platelet Rich Plasma Injections in Spine
Dextrose Injections in Spine
PICL Procedure at Regenexx, Colorado for CCJ ligament injections
Nerve Blocks
Physiotherapy
Upper Cervical Chiropractic (Atlas Orthogonal or NUCCA)
Chiropractic
Radiofrequency Therapies
Laser Therapy
Osteopathic and/or craniosacral therapy
List other treatments you have undergone for your brain and spine conditions
Other
/78
How satisfied are you with your Spinal Fusion surgery? (only respond if 1 year post- fusion surgery)

I did not have spinal fusion.
I had spinal fusion less than 1 year ago.
Extremely dissatisfied
Very dissatisfied
Somewhat dissatisfied
Neutral
Somewhat satisfied
Very satisfied
Extremely Satisfied
/78
How satisfied are/were you with your FIRST Regenerative Medicine SPINE Procedure? (only respond if 6 months post- treatment)
I did not have a regenerative medicine procedure.
I had a regenerative medicine procedure less than 6 months ago.
Extremely dissatisfied
Very dissatisfied
Somewhat dissatisfied
Neutral
Somewhat satisfied
Very Satisfied
Extremely Satisfied
/78
How satisfied are you with your Chiari Malformation posterior fossa decompression surgery?

I did not have posterior fossa decompression surgery
I had posterior fossa decompression surgery less than 3 months ago.
Extremely dissatisfied
Very dissatisfied
Somewhat dissatisfied
Neutral
Somewhat satisfied
Extremely Satisfied
/78
After Spinal Fusion or having completed Regenerative Medicine treatment, how much do you think your craniocervical junction disorder was a key contributor to your illness/symptoms?
I have not had fusion surgery nor regenerative treatments.
I think my craniocervical disorder contributed to none of my illness/symptoms.
I think my craniocervical disorder contributes to very little of my illness/symptoms.
I think my craniocervical disorder contributes to some of my illness/symptoms.
I think my craniocervical disorder contributes to a lot of my illness/symptoms.
I think my craniocervical disorder contributes to majority of my illness/symptoms.
I think my craniocervical disorder contributes to all of my illness/symptoms.
/78
State your level of agreement with the following statement. "I will be getting a full and comprehensive diagnosis and/or treatment of my spine and brain conditions in the next year".

Strongly Disagree
Disagree
Neutral
Agree
Stronly Agree
I already have had diagnosis and completed treatment
/78
State your level of agreement with the following statement. "I will recover from my illness and will resume a normal, disability free life".

Strongly Disagree
Disagree
Neutral
Agree
Agree
Stronly Agree
/78
State your level of agreement with the following statement. "I believe that the results of this survey will have a strong and positive impact on patient care for those with spine and brain conditions".

Strongly Disagree
Disagree
Neutral
Agree
Strongly Agree
/78
State your likelihood of getting a Multiple or 2nd Radiology Opinions on your imaging.

I do not have any Head and Neck imaging.
I already have a craniocervical disorder diagnosis and do not require a 2nd opinion.
Highly Unlikely
Unlikely
Unsure
Likely
Highly Likely
/78
Do you believe that Spine and Brain Advocate will be successful in assisting people get a spine and/or brain diagnosis and will help raise awareness and change in spine & brain related healthcare".

Highly Unlikely
Unlikely
Unsure
Likely
Highly Likely
/78
In 300 words or less, tell us about your illness onset and diagnostic and treatment journey.
/78
Orthostatic or Postural Hypotension is a form of low blood pressure that happens when you stand up from sitting or lying down. It can make you feel dizzy or lightheaded or faint. What is the frequency of your Orthostatic symtoms?
I never or rarely experience orthostatic symptoms when I stand up.
I sometimes experience orthostatic symptoms when I stand up.
I often experience orthostatic symptoms when I stand up.
I usually experience orthostatic symptoms when I stand up.
I always experience orthostatic symptoms when I stand up.
/78
What is the severity of your orthostatic symptoms?

I never experience orthostatic symptoms when I stand up.
I experience mild orthostatic symptoms when I stand up.
I experience moderate orthostatic symptoms when I stand up and sometimes have to sit back down for relief..
I never experience severe orthostatic symptoms when I stand up and frequently have to sit back down for relief. .
I experience severe orthostatic symptoms when I stand up and regularly faint if I do not sit back down..
/78
Under what conditions do your orthostatic symptoms occur?

I never or rarely experience orthostatic symptoms under any circumstances.
I sometimes experience orthostatic symptoms under certain conditions such as prolonged standing, a meal, walking or exposed to heat.
I often experience orthostatic symptoms under certain conditions such as prolonged standing, a meal, walking or exposed to heat.
I usually experience orthostatic symptoms under certain conditions such as prolonged standing, a meal, walking or exposed to heat.
I always experience orthostatic symptoms under certain conditions such as prolonged standing, a meal, walking or exposed to heat.
/78
How do you all of your symptoms interfere with your activities of daily living?

My symptoms do not interfere with activities of daily living (e.g work, chores, dressing, bathing)
My symptoms mildly interfere with activities of daily living (e.g work, chores, dressing, bathing)
My symptoms moderately interfere with activities of daily living (e.g work, chores, dressing, bathing)
My symptoms severely interfere with activities of daily living (e.g work, chores, dressing, bathing)
My symptoms severely interfere with activities of daily living and I am bedbound or wheelchair bound because of my symptoms.
/78
What is the current status of your illness? (Karnovsky Scale)

100% Normal, no complaints or evidence of disease
90% Able to carry on normal activities; minor signs or symptoms of disease
80% Normal activities but with effort. some signs and symptoms of disease
70% I care for myself, but I am unable to carry on normal activities or do active work.
60% I require occasional assistance but I am able to care for most of my needs.
50% I require considerable assistance and frequenct medical care.
40% I am disabled and require special care and assistance
30% I am severely disabled and hospitalization is indicated but death is not imminent
20% I am hospitalized, very sick and active life support is necessary
10% Fatal processes are progressing rapidly
/78
In your opinion, who are the world's leading expert on Spine and Brain Disorders for DIAGNOSIS AND TREATMENT?

Dr. Fraser Henderson
Dr. Gilete
Dr. Paolo Bolognese
Dr. Sunil Patel
Dr. Centeno
Dr. Schultz
Dr. Pitts
Other
Other
/78
I have been formally diagnosed by a CCI expert.
Yes
No
I have not consulted with a CCI expert.
/78
Select the one that best describes your symptoms.
I have headaches, upper neck pain, dissiness, imbalance, lightheadedness, brain fog and cracking in the neck
I have headaches, upper neck and shoulder pain, dizziness, brain fog, cracking in the neck, ringing in the ears, rapid heart rate, jaw pain, numbness/tingling in various body parts, fatigue, nausea, migraines
I have facial pain, tongue numbness or spasms, loss of consciousness, neck & shoulder pain, dizziness, brain fog, cracking in neck, ringing in the ears, rapid heart rate, jaw pain, various body part numbness/tingling, fatigue, nausea, cannot be upright
None of the above
/78
Select the answer that best describes what relieves your symptoms.

I have temporary relief of symptoms from neck physiotherapy.
I have temporary relief of symptoms from neck massage.
I have temporary relief of symptoms from NUCCA chiropractic.
I have temporary relief of symptoms from Atlas Orthogonal chiropractic.
All or most of the treatments above temporarily relieve my symptoms
None of these treatments relieve my symptoms, even on a temporary basis.
I have not tried any of these treatments.
/78
In your own opinion, what imaging do you believe is the best imaging for helping to diagnose craniocervical instability?

Davis XRay Series
Flexion and Extension XRays
Dynamic Digital Motion XRay with CCJ Experts
Dynamic Digital Motion XRay
Upright flexion and extension MRI
Supine MRI 1.5T or 3T
CT Scan (static)
CT Scan dynamic/rotational
I don't know or don't have an opinion
/78
If a progressive treatment path for upper cervical instability includes the steps: 1. Conservative (physio, osteopath, chiro, meds etc.) 2. Posterior PRP injections 3. PICL and 4. Fusion... what step are you at currently in the process?

Conservative treatment / management
Posterior PRP Injections
PICL
Fusion / Surgery
/78
What is your current opinion on Regenerative / Orthobiologics Medicine? Select one that best describes your current beliefs.

It's a medical hoax / false treatment / joke
The risks outweighs any benefits of treatment
The science is still too "experimental" for me and I will wait and see
I know it's experimental and has risks but the potential benefits of treatment outweigh not trying orthobiologics
I have or would try PRP but still think stem cells are too early / experimental to try
I plan to have orthobiologics in the next year; and have confidence it will help me achieve a better quality of life but I have some concerns about the adverse events of the procedure.
I plan to have orthobiologics in the next year; and have confidence it will help me achieve a better quality of life and have no concerns about the adverse events of the procedure.
I have had orthobiologics and have no regrets - my quality of life is better.
I have had orthobiologics and my quality of life is the same - I saw no improvements.
I have had orthobiologics and have a worse quality of life that I believe is directly from the orthobiologics procedure.
/78
Which of the following statements best apply to you.

I never wear a cervical collar because I was told not to by a heathcare practitioner.
I wear a hard cervical collar some of the time.
I wear a hard cervical collar all of the time because I believe it helps me function better.
I wear a hard cervical collar all of the time because I have to wear it in order to survive or function.
I wear a soft cervical collar some of the time.
I wear a soft cervical collar all of the time because I believe it helps me function better.
I wear a soft cervical collar all of the time because I have to in order to survive or function.
I never wear a cervical collar because it did not relieve my symptoms.
/78
Select the statements that most closely applies to your situation.

I have a normal cervical spine c-shaped curve.
I have an abnormal cervical spine c-shaped curve.
I have been formally diagnosed with kyphosis.
I have improved my cervical spine curve with curve restoration therapy.
I have or am trying to improve my cervical spine curve at home with the help of home traction devices, therapy pillows and/or maintaining proper postural positions while on an electronic device or watching TV etc.
I have tried curve restoration therapy with a healthcare provider or at home but it didn't improve my cervical spine curve.
I don't have a diagnosis or information about my spinal curve
/78
Select the spine / neck treatments that you have tried and best describe how they have helped you. Select all that apply.

I have tried occipital nerve blocks and they did not help relieve my pain.
I have tried occipital nerve blocks and they helped relieve my pain.
I have tried pulsed radiofrequency neuromodulation and it did not help relieve my pain.
I have tried pulsed radiofrequency neuromodulation and it did helped relieve my pain.
I have tried facet medial branch blocks and it did not help relieve my pain.
I have tried facet medial branch blocks and it did helped relieve my pain.
I have tried medial branch radiofrequency ablation and it did not help relieve my pain.
I have tried medial branch radiofrequency ablation and it did help relieve my pain.
I haven't tried any of the treatments listed above.
Other
/78
Select the answer that best describes your current position with PICL procedure.
I do not know what PICL procedure is.
I know about the PICL procedure but am chosing or have chosen a conservative path.
I know about the PICL procedure but am chosing or have chosen fusion surgery..
I have had 1 PICL procedure.
I have had 2 PICL procedures
I have had 3 PICL procedures
I have had 4 PICL procedures
/78
For those that have had surgery, select the answers that best describe your situation.

I have not had any fusion, decompression or styoidectomy procedure.
I have had fusion surgery and it has helped my symptoms and quality of life.
I have had fusion surgery and it has not helped my symptoms and quality of life.
I had fusion surgery done in Canada.
I had fusion surgery done in USA.
I had fusion surgery done outside of North America.
I had decompression surgery and it has helped my symptoms and quality of life.
I had decompression surgery and it has not helped my symptoms and quality of life.
I had decompression surgery in Canada.
I had decompression surgery in USA.
I had decompression surgery done outside of North America.
I have had styloid surgery and it has helped my symptoms and quality of life.
I have had styloid surgery and it has not helped my symptoms and quality of life.
I had styloid surgery in Canada.
I had styoid surgery in USA.
I had styoid surgery outside of North America.
I need surgery and am on a waitlist.
I cannot get a referral to a specialist but suspect I need surgery.
I had decompression surgey that did not relieve my symptoms and later was diagnosed with craniocervical / atlantoaxial instability.
I was fused C1-C2
I was fused C0 (occipital) to cervical spine
/78
Select the answer that best describes your knowledge of craniocervica junction disorders and their treatments.

0 - this is new to me and I have a lot to learn
1 - I am somewhat familiar but need a lot of help and guidance
2 - I have confidence that I know enough to get through this successfully
3 - I understand all key elements and can apply it to me
4 - I understand all key elements and can teach others or write a book
/78
Through radiology reports or CCI expert, describe your CXA in flexion?
Abnormal
Borderline
Normal
I haven't investigated
/78
Through radiology reports or CCI expert, describe your CXA in extension?
Abnormal
Borderline
Normal
I haven't investigated
/78
Through radiology reports or CCI expert, describe your Grabb-Oakes in flexion?
Abnormal
Borderline
Normal
I haven't investigated
/78
Through radiology reports or CCI expert, describe your Grabb-Oakes in extension?
Abnormal
Borderline
Normal
I haven't investigated
/78
Through radiology reports, did your Grabb-Oakes measurement from Neutral to Flexion change?
No change in Grabb-Oaks neutral and flexion measurements
There was less than 2 mm change in my Grabb-Oakes measurement between neutral and flexion positions
There was 2 mm - 3.9 mm change in my Grabb-Oakes measurement between neutral and flexion positions
There was less 4 mm - 5.9 mm change in my Grabb-Oakes measurement between neutral and flexion positions
There was greater than 6mm change in my Grabb-Oakes measurement between neutral and flexion positions
/78
I have a sacral dimple. A sacral dimple is an indentation or pit in the skin on the lower back that is present at birth. It's usually just above the crease between the buttocks.
Yes
No
I don't know.
/78
I don't have a diagnosis of tethered cord but... select the answer that most closely applies to you.
I have a diagnosis of tethered cord or I had a diagnosis of tethered cord and had surgery.
I do not have the diagnosis of tethered cord but have the symptoms: constant back and leg pain, which may extend to the rectum and genital area in some cases AND other signs of tethered cord such as sacral dimple, fatty deposit and thickened filum on MRI Lumbosacral
I do not have neither of the above.
/78
Is there anything else you'd like to add? Please write your answer here.
/78
In 3 words, describe your healthcare journey.
THANK YOU!
We appreciate you taking the time to complete this survey! Once we have enough data, we will share results on Spine and Brain Advocate's website. Once we have enough data to provide substantial evidence to create a case for change, we will be lobbying for changes to healthcare for Craniocervical Junction Disorder patients. Stay tuned!
