OMI QUIZ # 2. How good are you at diagnosing OMI? Can you outperform the Queen?
This quiz contains a total of 27 ECGs. All ECGs are from patients presenting with chest pain. Your job is to determine whether or not the ECGs represent occlusion myocardial infarction (OMI) and whether or not the cath lab should be activated. All ECGs 25mm/s
I've included in the desription above each ECG a link to a higher resolution image.
Good luck!

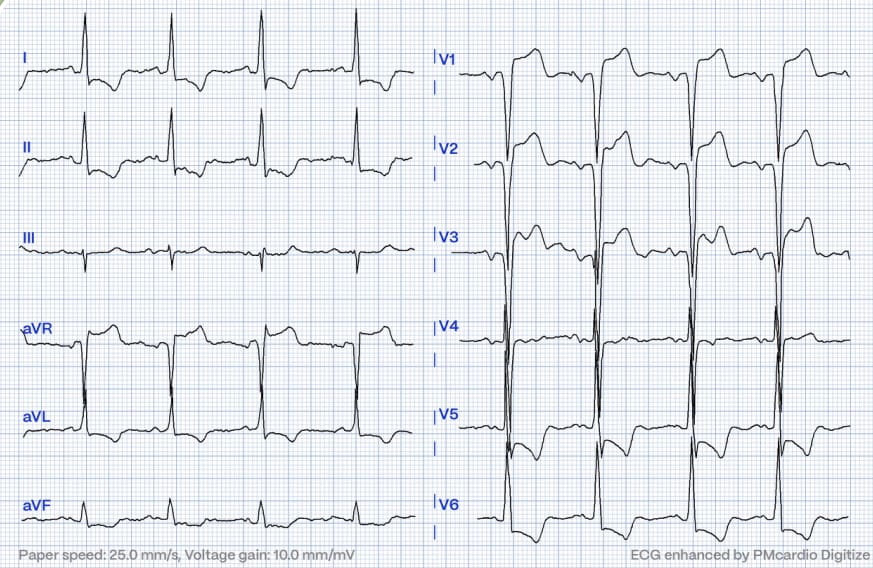
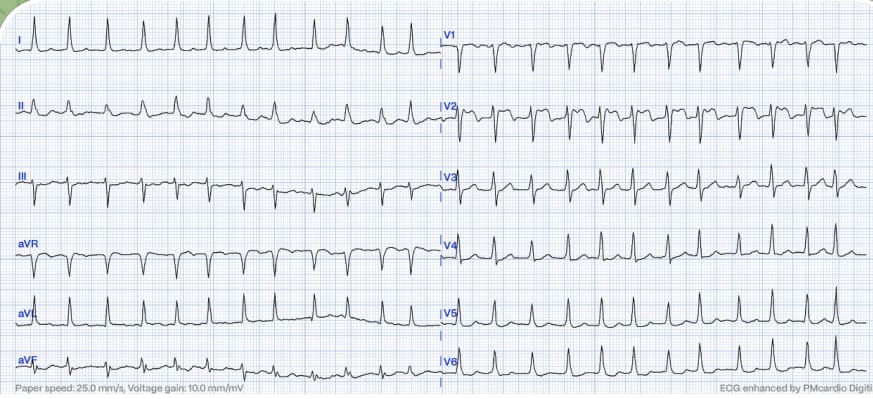
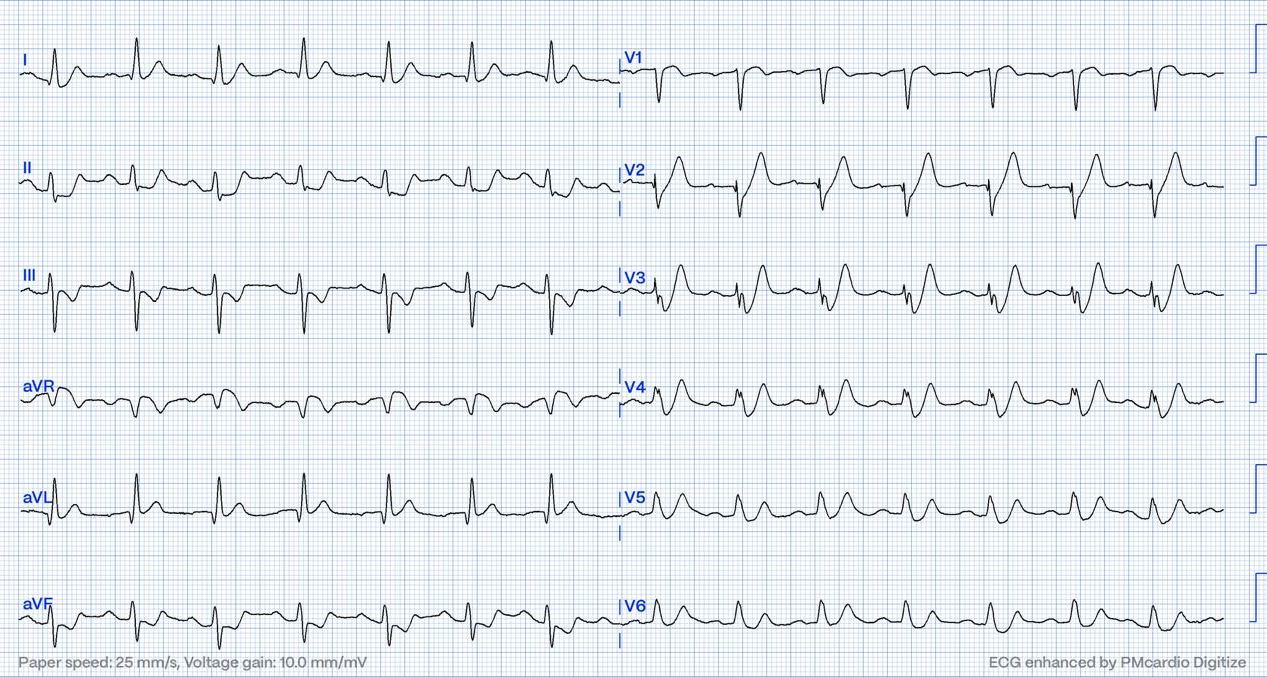
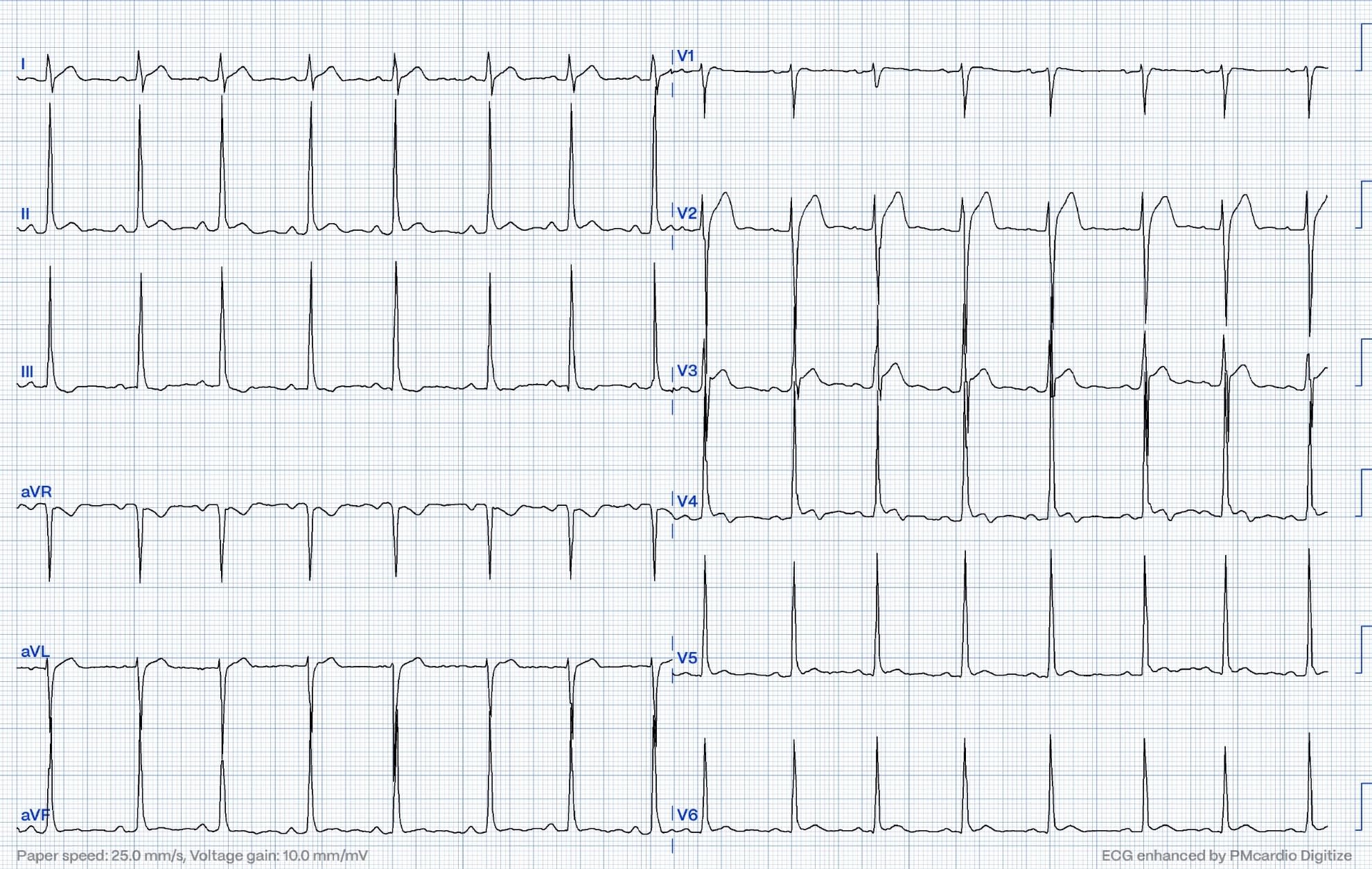
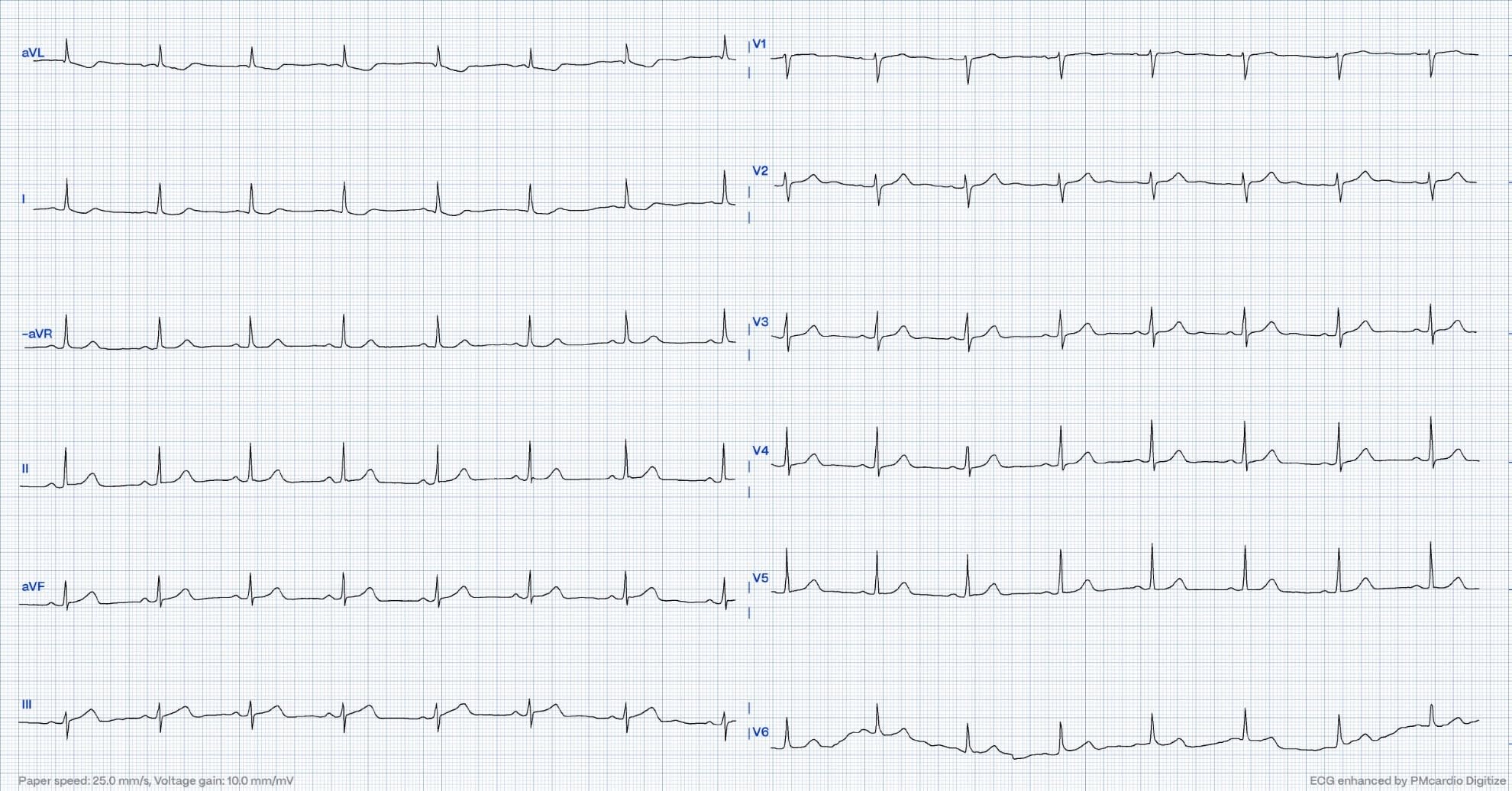
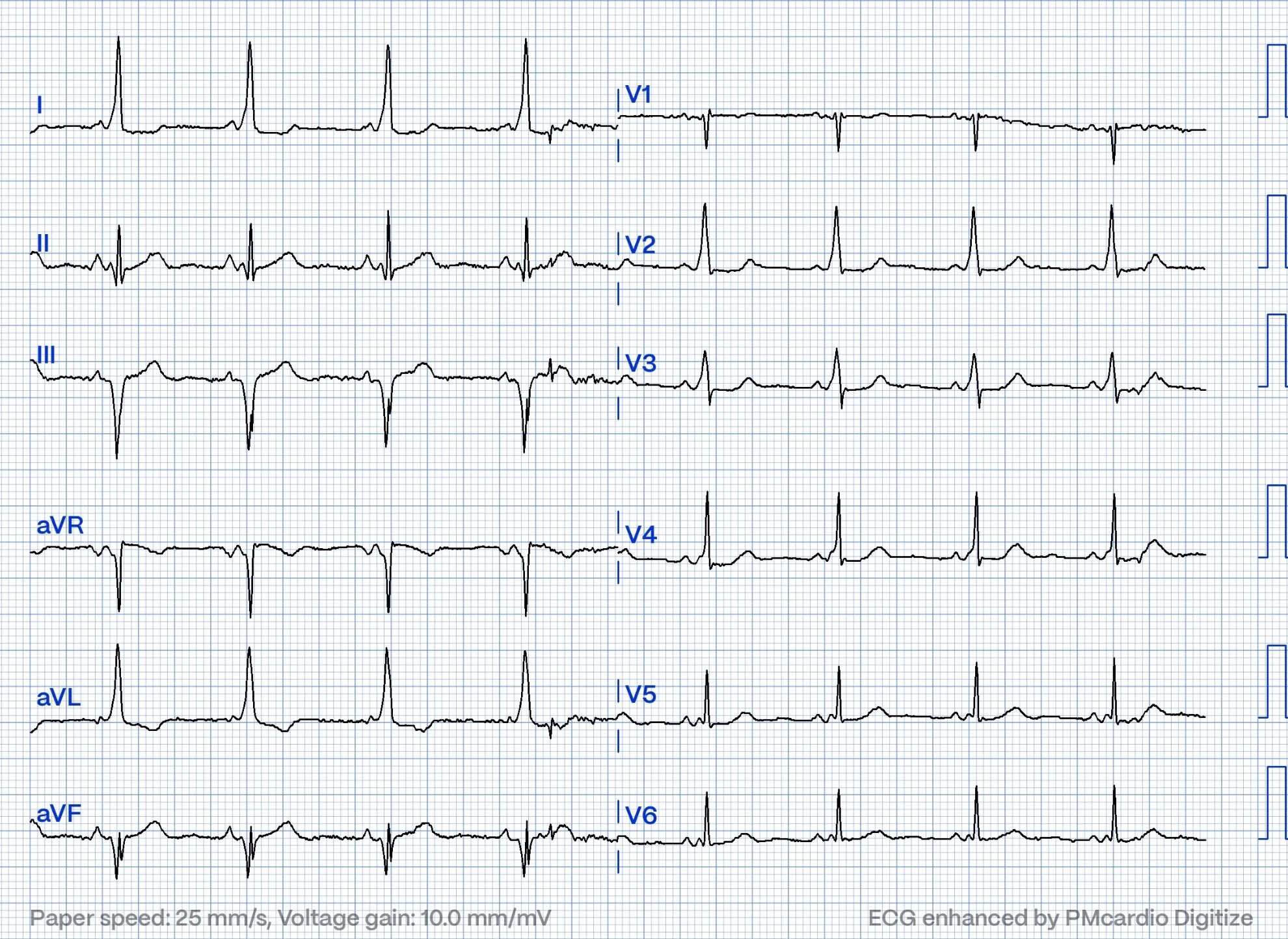
Case 1

This is early repolarization. Some providers maybe would suspect pericarditis here. There is no Spodnik sign (PR-segment depression) There are well formed J-waves and a low ST/T ratio. This patient had an angiogram done that was negative. Troponins undetectable.
QoH: NOT OMI HIGH CONFIDENCE
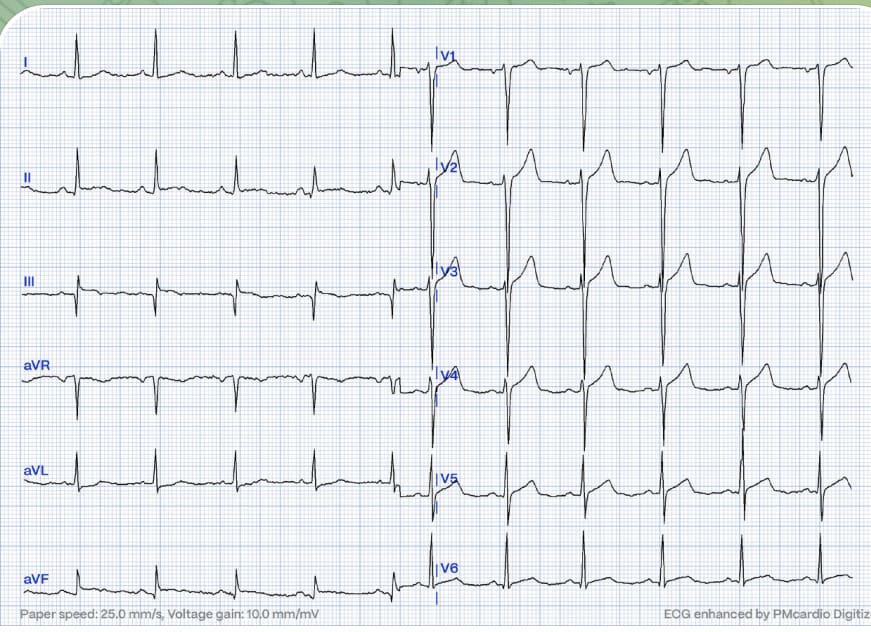
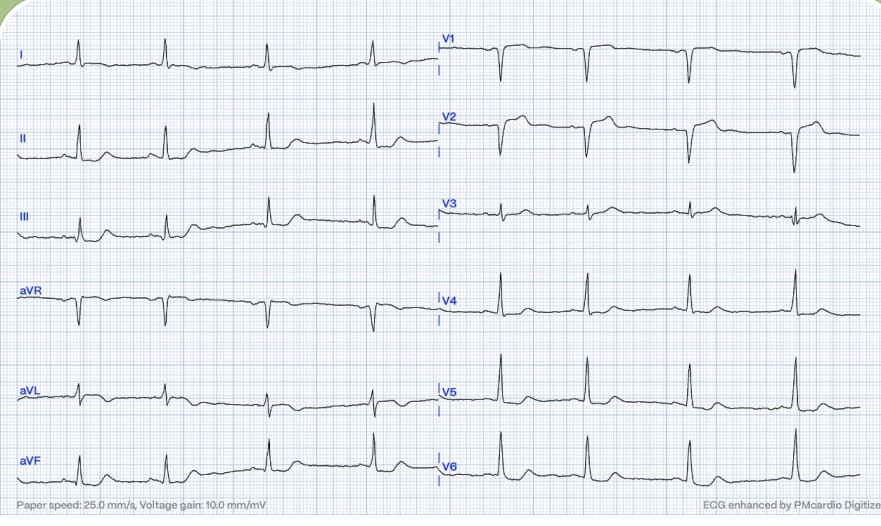
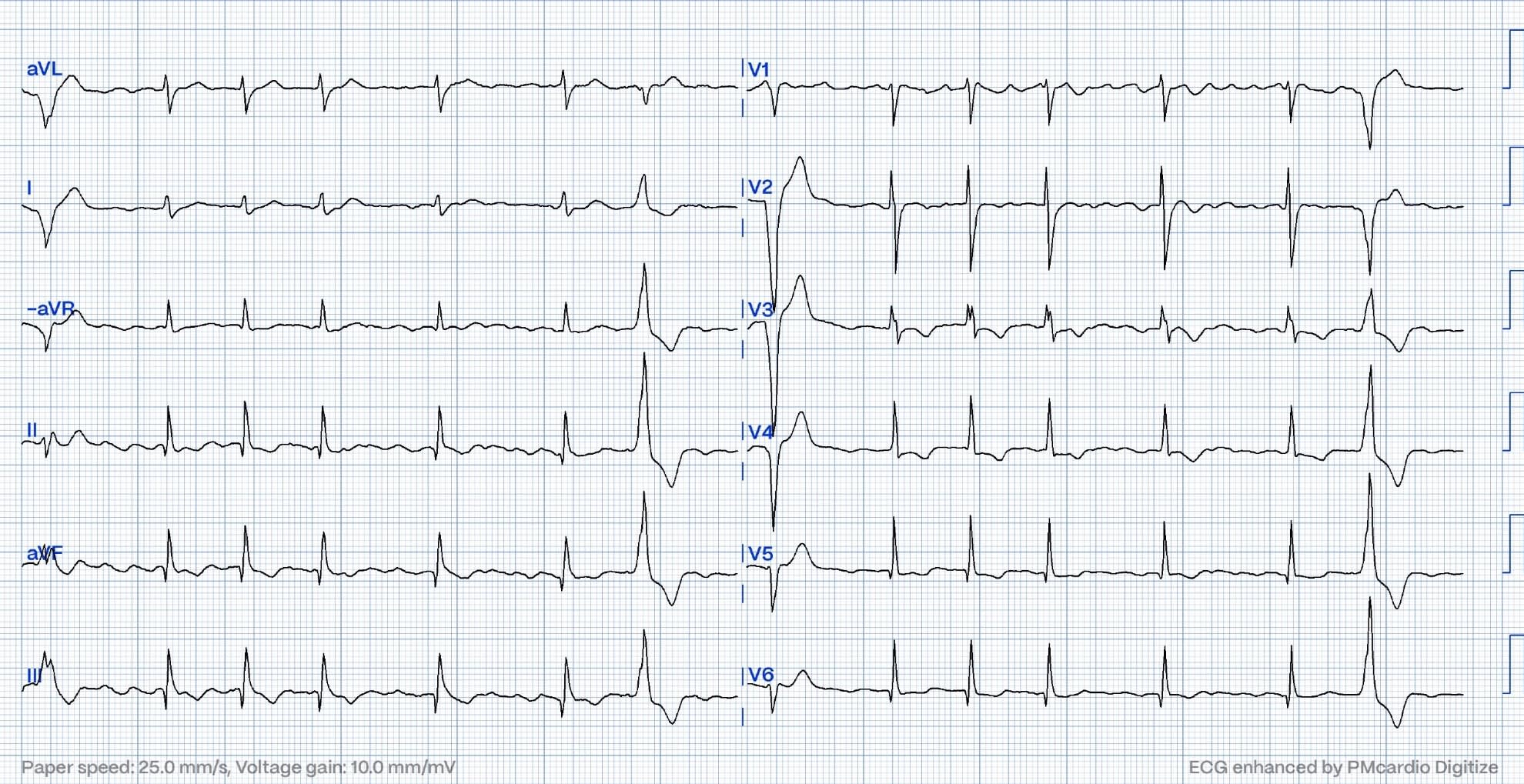
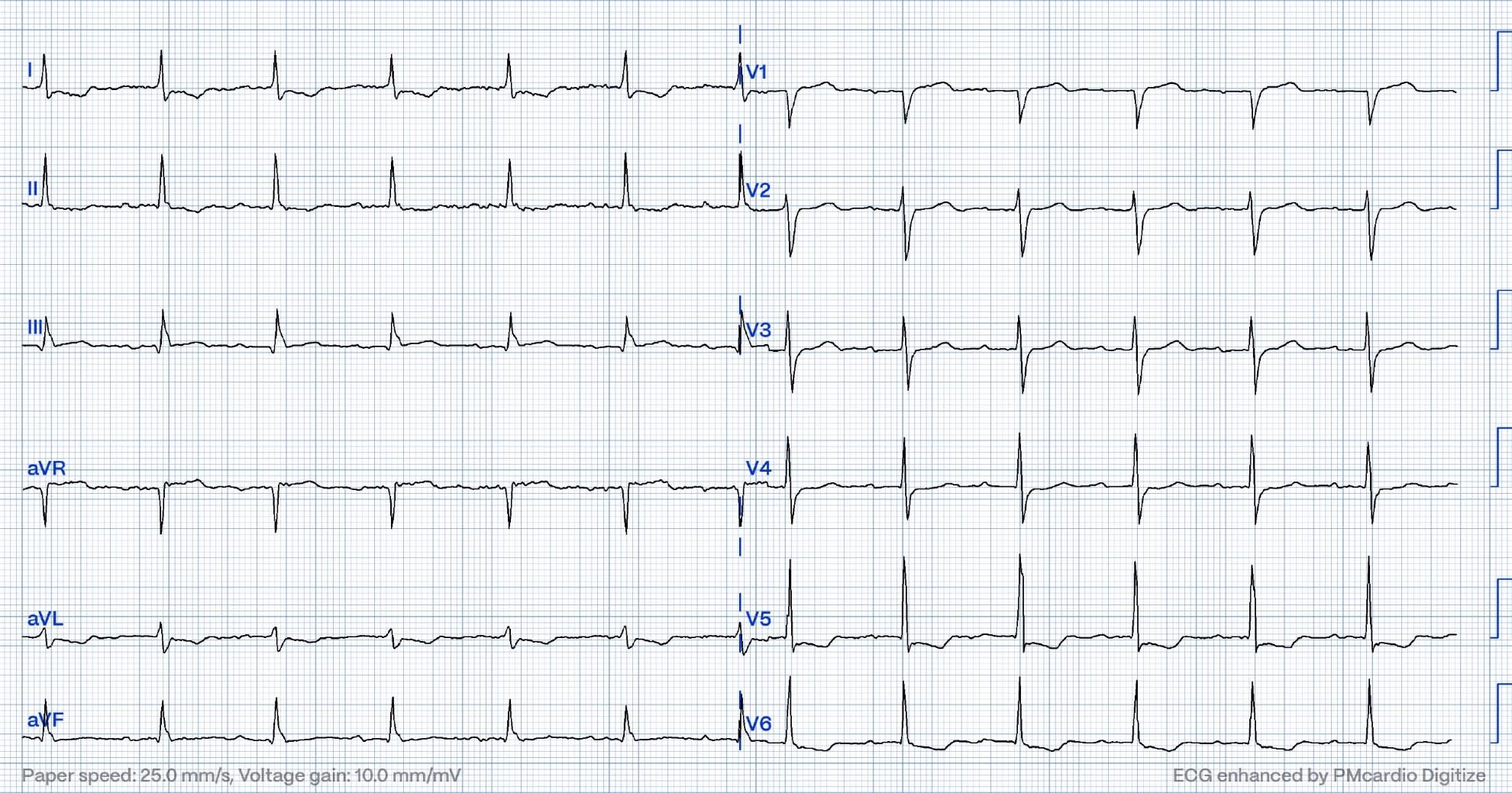
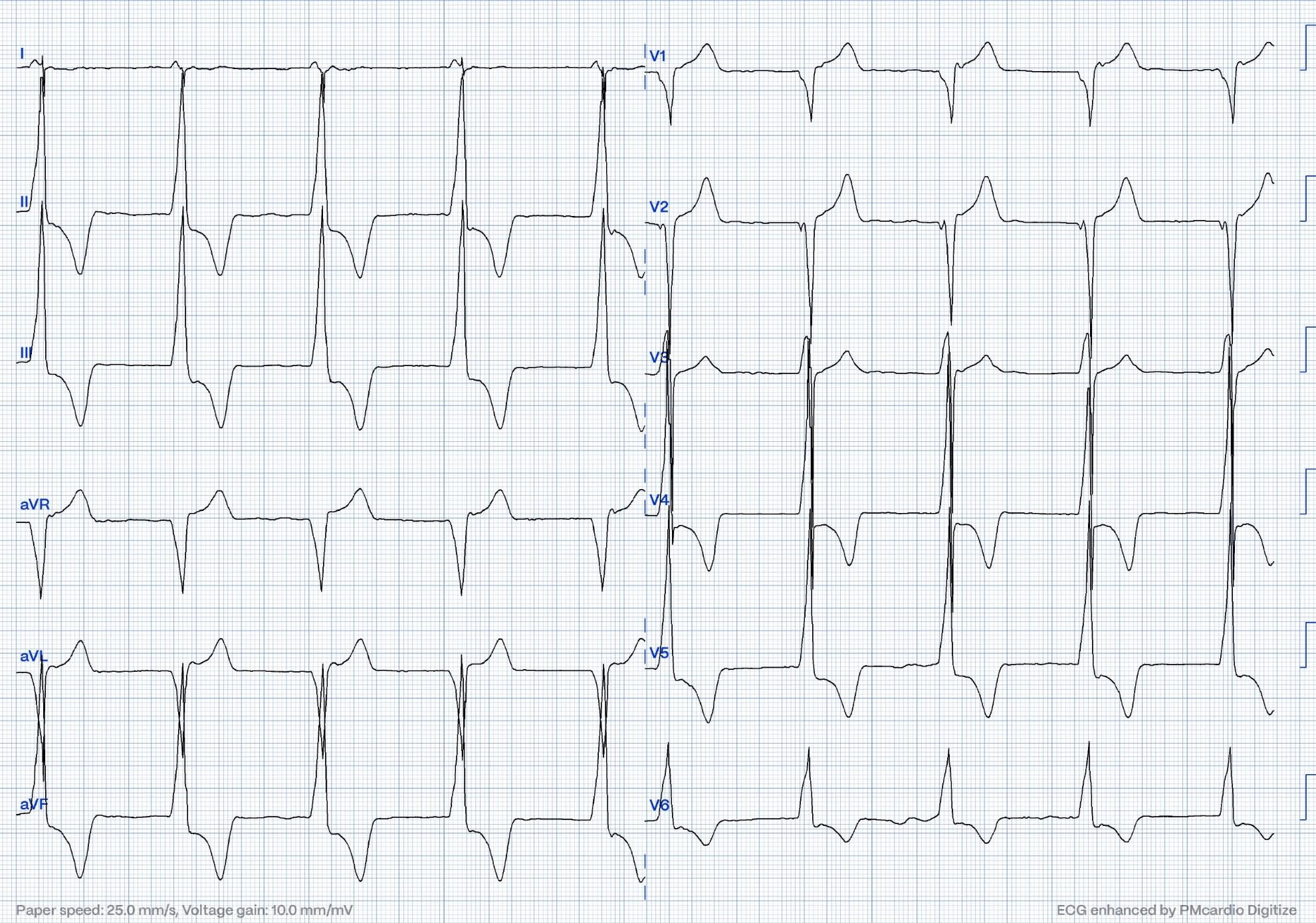
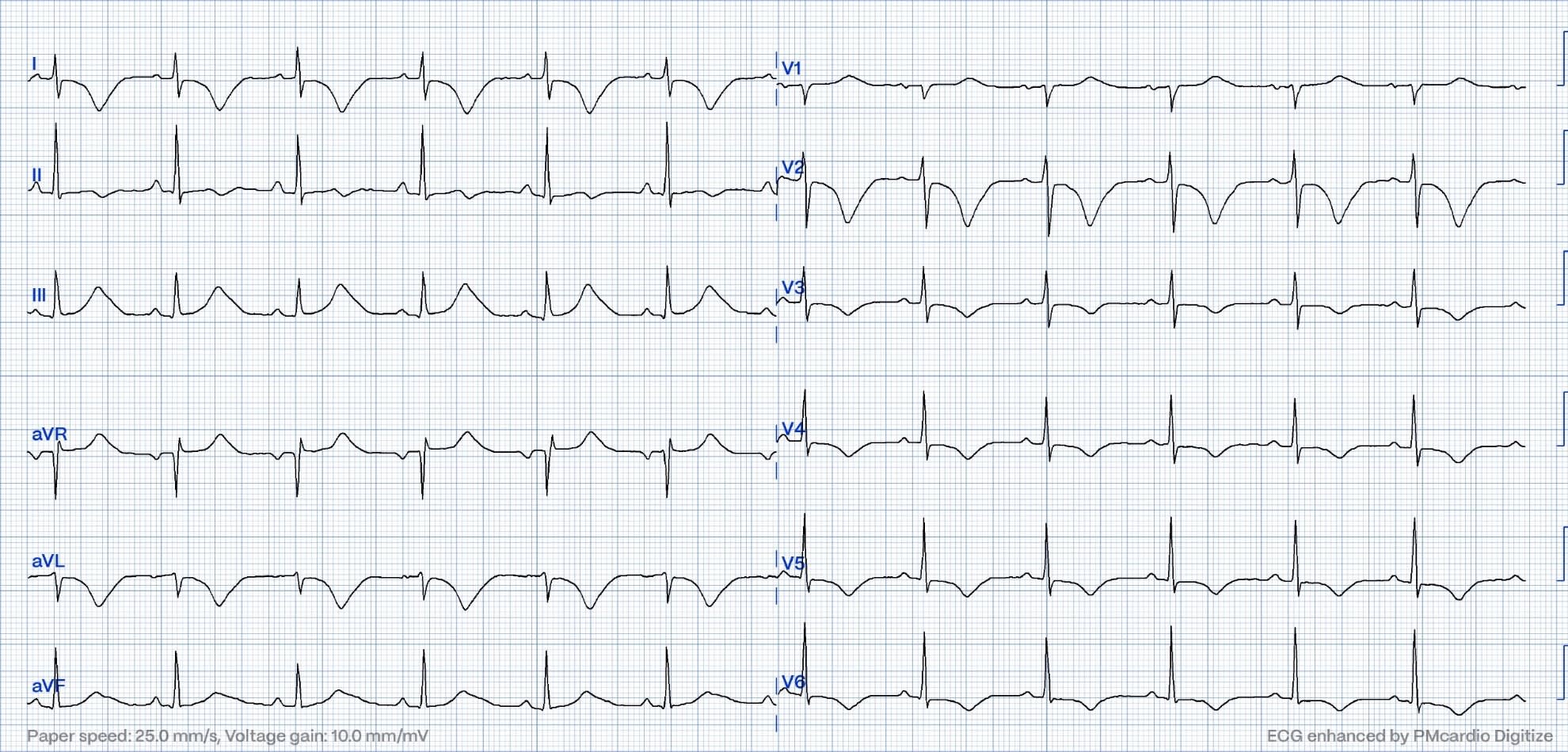
Case 2
This ECG shows LVH in combination with subendocardial ischemia. The patient had CKD stage 5 and anemia. Troponins were slightly elevated without significant change. ST depression vector is maximal in lead V5
QoH NOT OMI HIGH CONFIDENCE
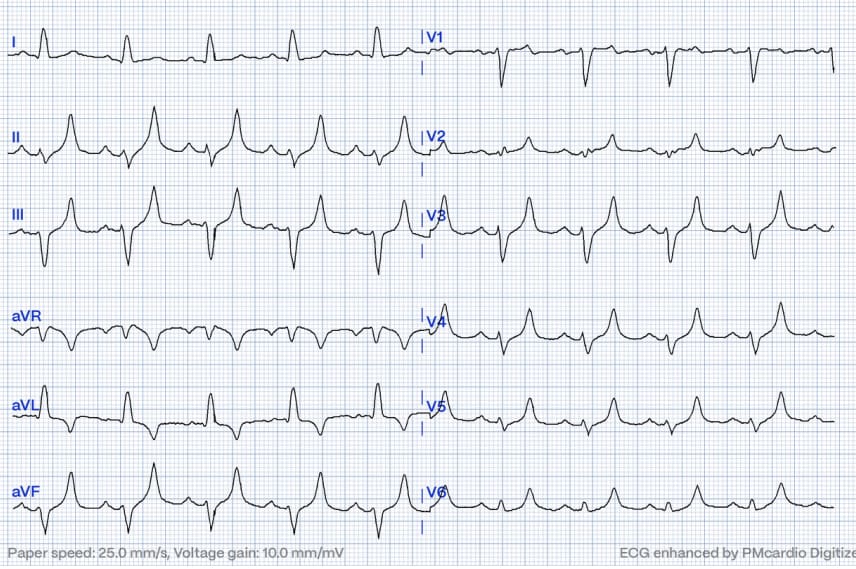
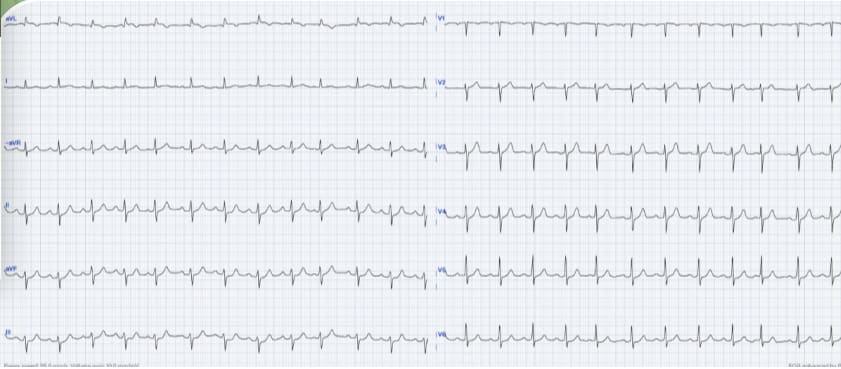
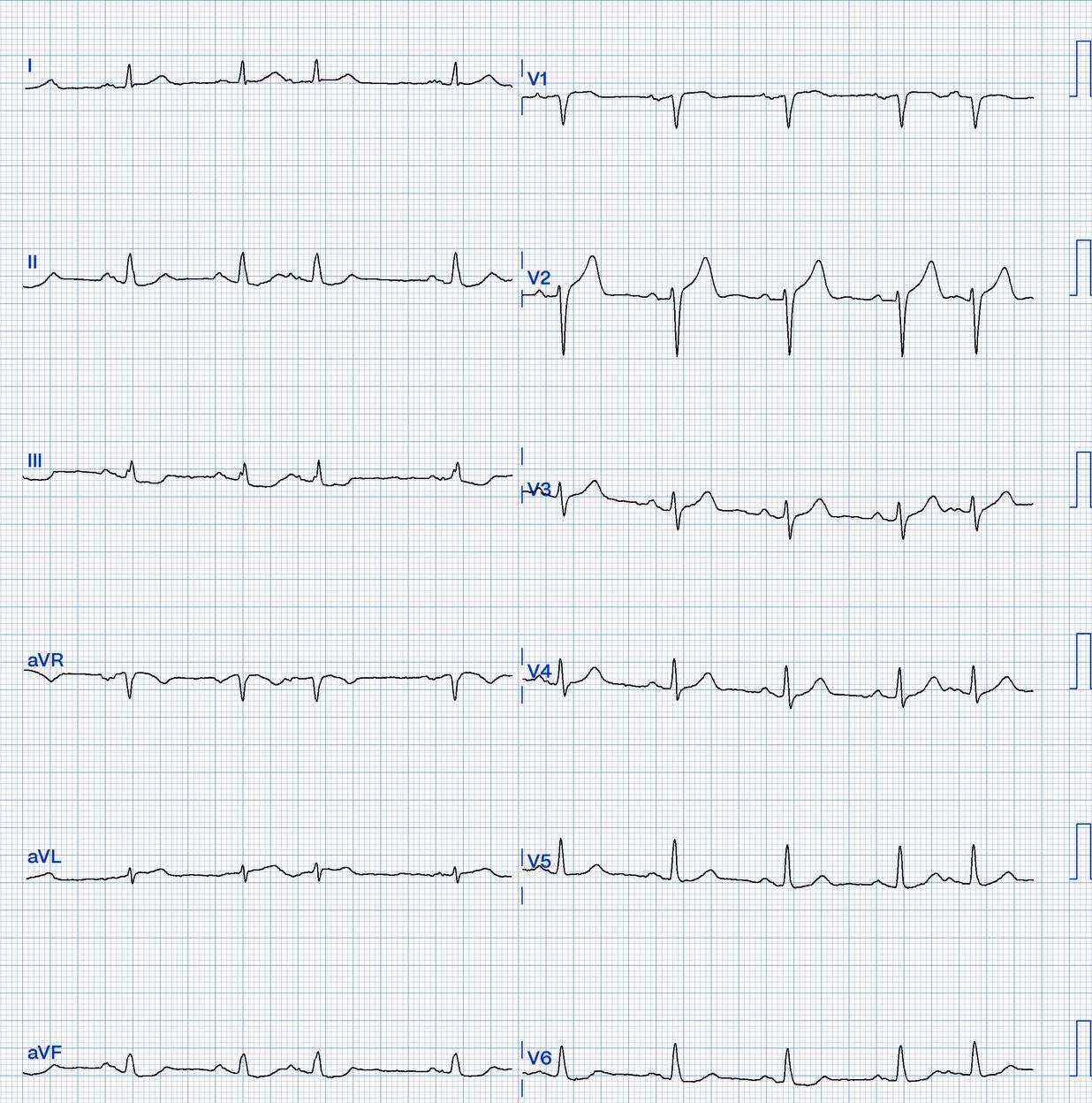
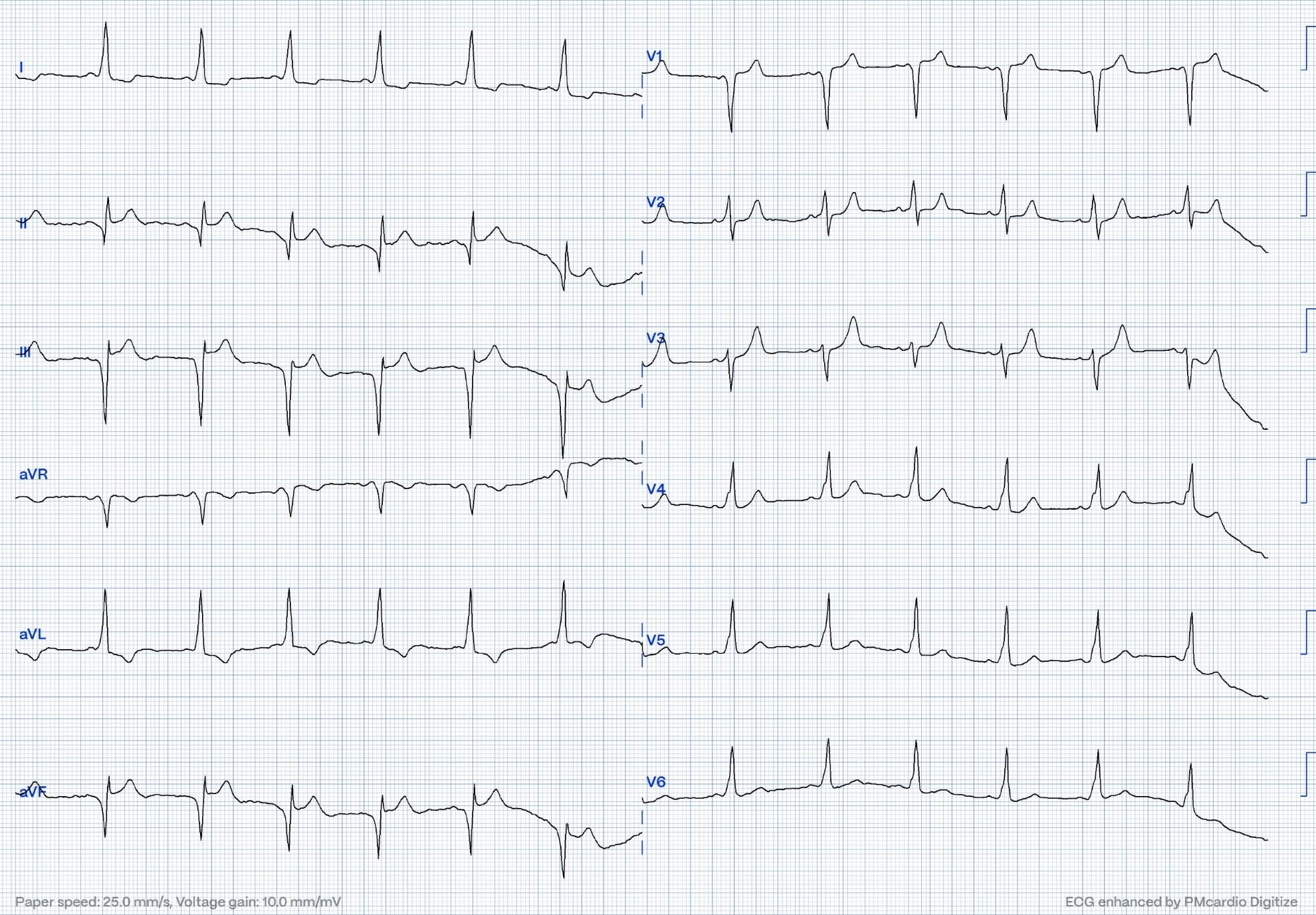
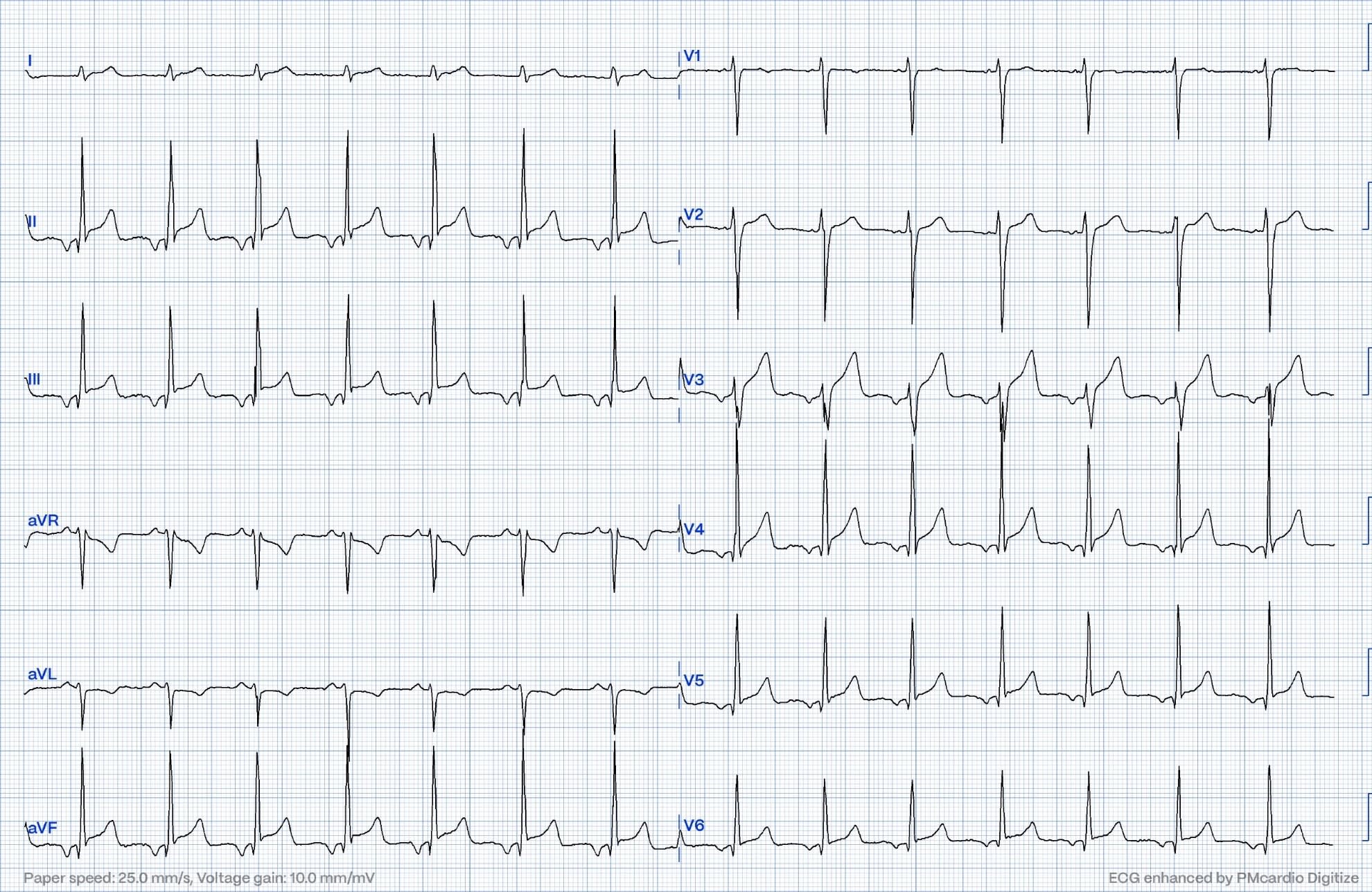
Case 3
This ECG shows findings consistent with occlusion myocardial infarct (OMI). There was occlusion of a distal LAD that supplied parts of the inferior wall. Type III "wrap-around" LAD. Notice the slight ST elevation in the inferior leads and hyperacuteness of the T wave in V4.
QoH OMI HIGH CONFIDENCE
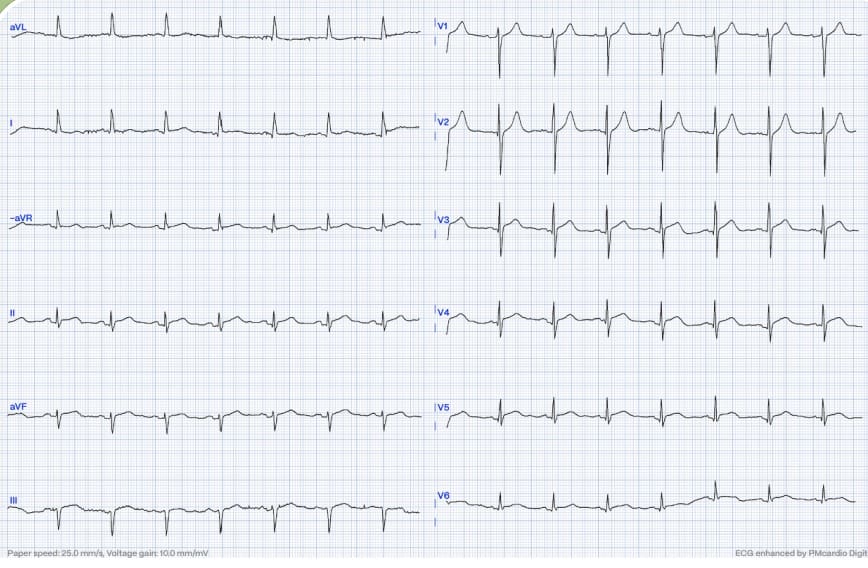
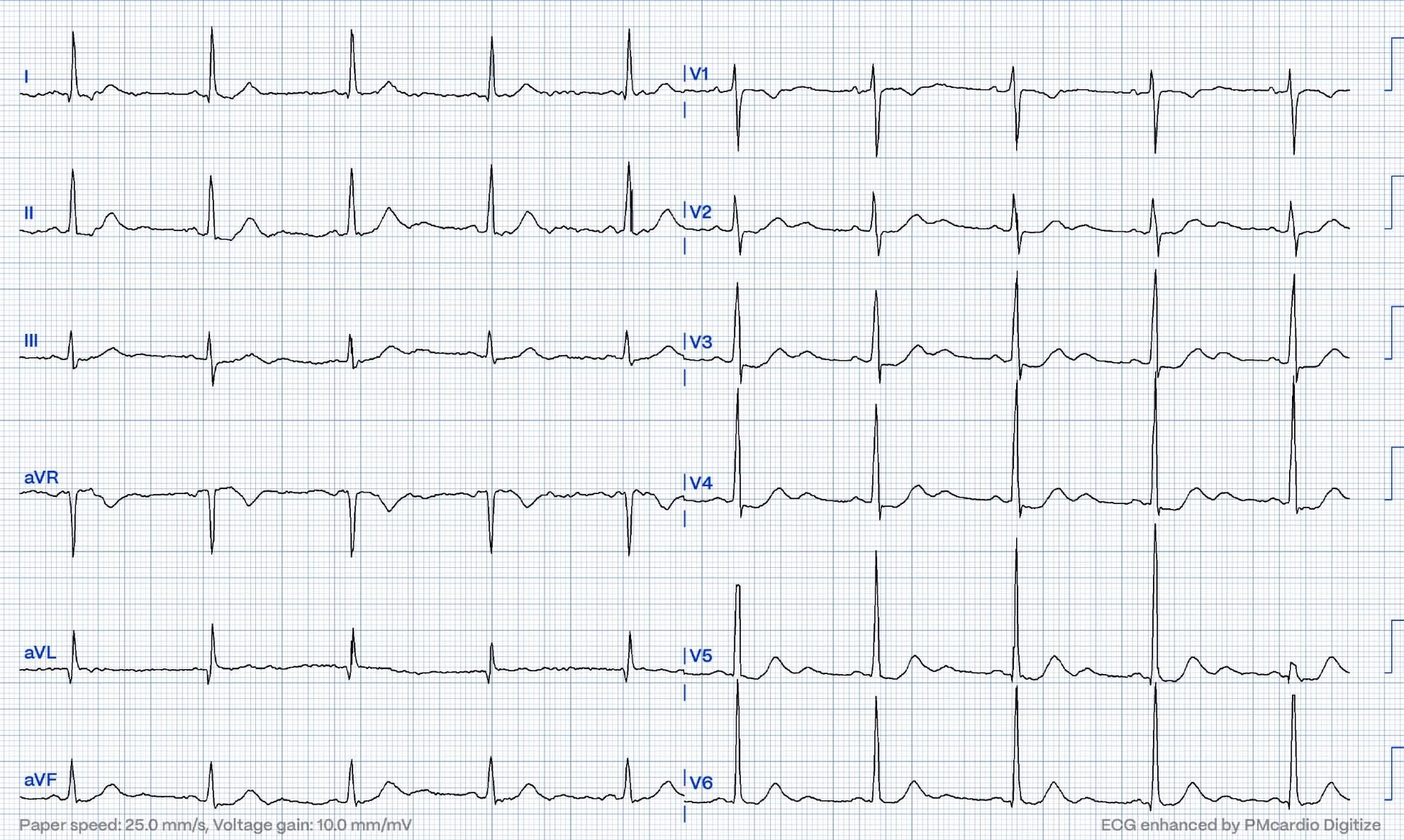
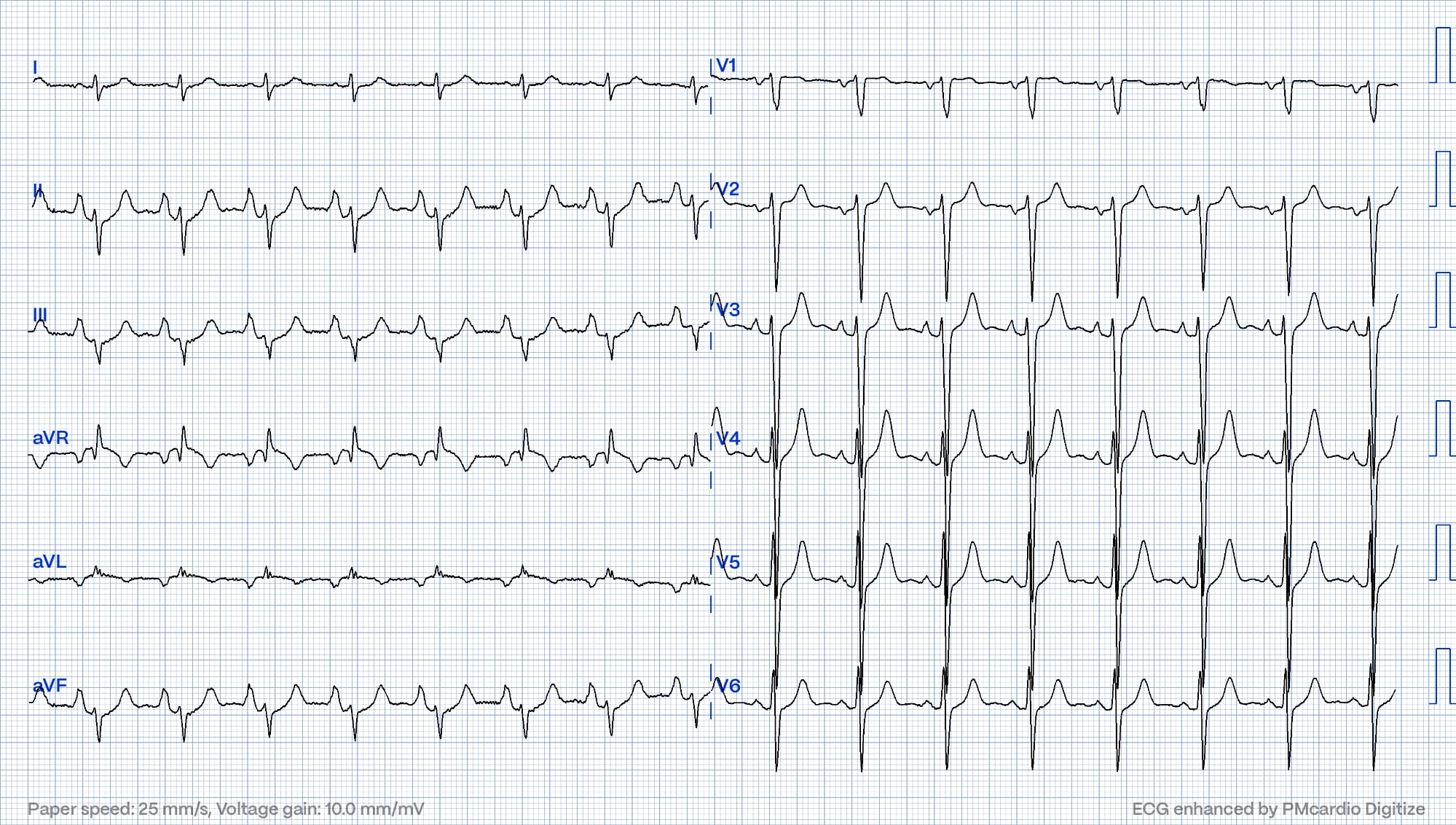
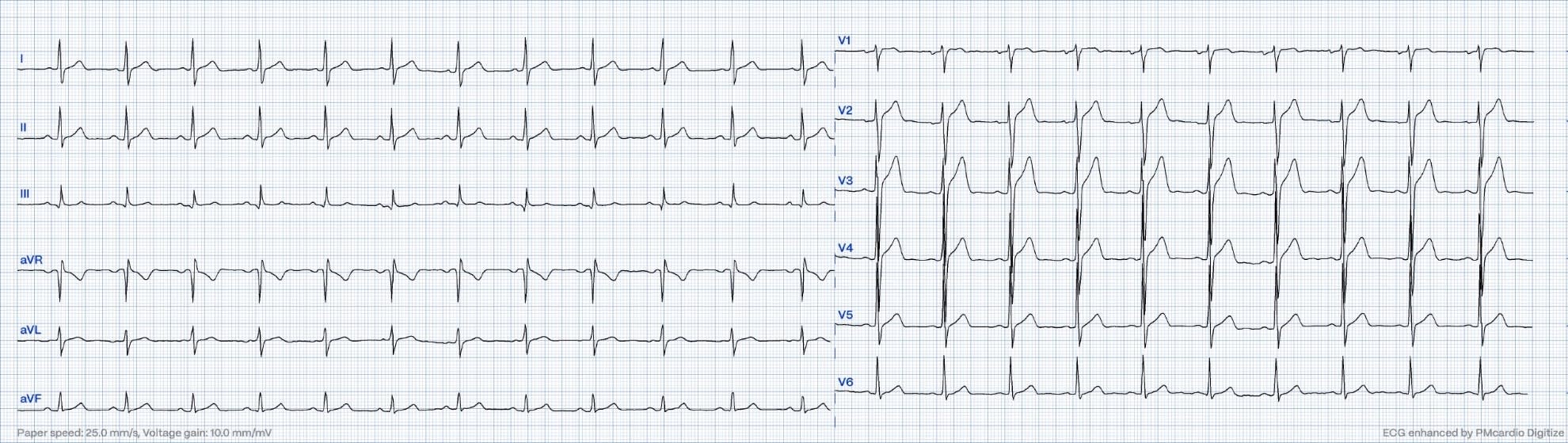
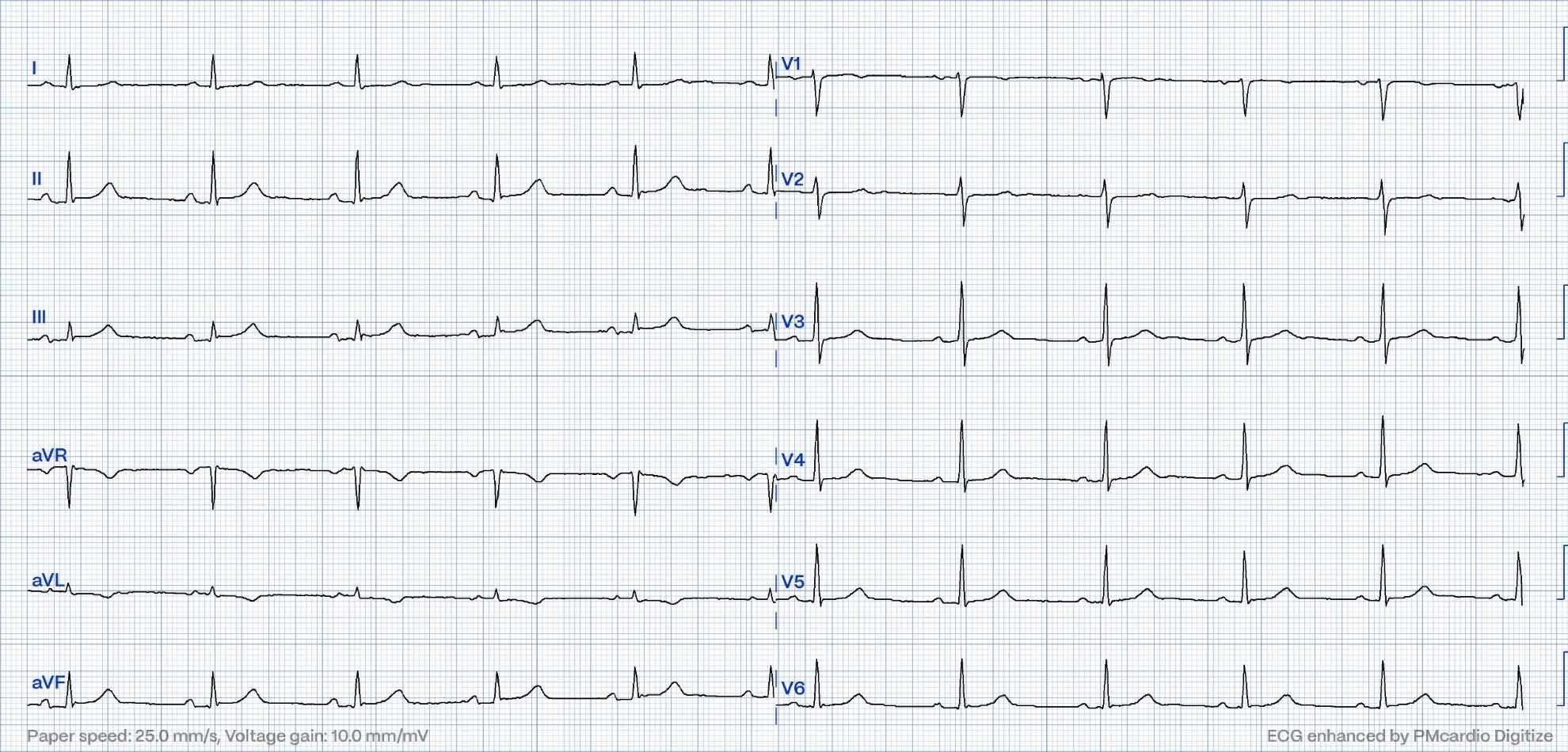
Case 4
This ECG is pathognomonic for severe hyperkalemia. Hyperkalemia can give profound ST-T changes that can mimic acute myocardial infarction. The narrow base, peaked T waves in this ECG is not consistent with OMI. Potassium measured 8,1
QoH NOT OMI HIGH CONFIDENCE
Case 5
This patient's angiogram showed mild disease in the mLAD. TIMI III flow. Troponin T peaked above 1500ng/L well in the range of STEMI/OMI. The ECG was recorded during chest pain. Clinical picture and ECG consistent with a lyzed thrombus
QoH OMI HIGH CONFIDENCE
Case 6

This ECG is very concerning and diagnostic of anterior wall occlusion myocardial infarct (OMI). There is RBBB and LAH. Both were new. New bifascicular block in conjuction with anterior wall MI carries a bad prognosis. This patient developed cardiogenic shock with a huge troponin value. Troponin T >19.000 ng/L
QoH OMI HIGH CONFIDENCE
Case 7

This ECG shows sinus rhythm with "shark fin" ST elevation. What appears to be wide QRS complexes are infact not. The QRS complexes are narrow with massive ST elevation. Look at V1 and imagine a vertical line from the J point through the precordial leads. The STE becomes apparent! Extensive anterior wall OMI!
QoH OMI HIGH CONFIDENCE
Case 8
This ECG shows atrial fibrillation with RVR. There is ST elevation in V2. The morphology is not typical of ischemia. Infact this patient was on flecainide and it turned out that the flecainide unmasked Brugada morphology. The patient had cardiac arrest shortly after this ECG was recorded. Angiogram was negative and troponins barely elevated from the arrest. ECG changes slowly disappeared after flecainide discontinuation.
QoH NOT OMI HIGH CONFIDENCE
Case 9

This ECG is also an example of hyperkalemia.
QoH NOT OMI HIGH CONFIDENCE
Case 10
This ECG is consistent with LAD occlusion. "Precordial swirl" pattern. pLAD occlusion.
QoH OMI HIGH CONFIDENCE
Case 11
This patient had an occluded marginal branch of the LCx. Notice the slight ST coving and T inversion i aVL with reciprocal changes in the inferior leads. The Queen caught these subtle findings.
QoH OMI MID CONFIDENCE
Case 12
This was severe pLAD disease/subtotal occlusion. There is ST depression in several leads. The ECG represents SEI (subendocardial ischemia) in the setting LAD disease. Sometimes SEI can be difficult to differentiate from eg posterior OMI and this ECG could easily have represented posterior OMI
QoH OMI HIGH CONFIDENCE
Case 13
This ECG is diagnostic of a total or subtotal proximal LAD occlusion. The ECG is very pathologic despite having zero ST elevation. This is textbook DeWinter T waves. Troponin T peaked at nearly 9000ng/L.
QoH OMI HIGH CONFIDENCE
Case 14
This ECG is from a patient with ARVC. The ST-T changes here are not due to ischemia.
QoH NOT OMI HIGH CONFIDENCE
Case 15

This ECG shows atrial flutter with complete heart block and narrow escape rhythm. There is also an inferoposterior OMI. This patient was very elderly. The patient was managed conservatively. Peak Troponin I > 150.000ng/L (!)
QoH OMI HIGH CONFIDENCE
Case 16
LAD occusion unrecognized by provider. Delayed cath lab activation. Large troponin release. Troponin T > 7000ng/L. Delay could have been avoided with the Queen of hearts.
QoH OMI HIGH CONFIDENCE
Case 17
This ECG shows ST depression in the inferior leads and slight STe with T inversion i aVL. One could be tricked into thinking this was a high lateral OMI with reciprocal ST depression. It is not. The P waves are of significant magnitude. The ST depression in the inferior leads is caused by atrial repolarization. (Ta wave) This is atrial repolarization mimicking OMI. A very tricky ECG. Troponins were normal on presentation and on repeat blood test.
I thought the QoH would be fooled by this ECG. She was not!
QoH NOT OMI HIGH CONFIDENCE.
Case 18
This ECG shows benign T wave inversion. (BTWI) This is a normal variant of ST elevation. This ECG lead to a false positive Cath lab activation. Normal coronaries. Normal troponins. The Queen of Hearts understands that this is not an acute coronary occlusion.
QoH NOT OMI HIGH CONFIDENCE
Case 19
This ECG shows widespread ST depression with ST vector towards V5 (maximal ST depression here). An ST vector towards lead V5 is consistent with sudendocardial ischemia (ref case # 2). However, this ECG shows Aslangers pattern as there is ST-elevation in lead III, this makes it a STEMI equivalent. The Queen knows that this is not simple subendocardial ischemia.
QoH OMI HIGH CONFIDENCE
Case 20
This ECG is a nice example of pseudoinfarct pattern from WpW. Here the preexcitation mimics inferoposterior transmural ischemia.
QoH NOT OMI HIGH CONFIDENCE
Case 21
This is normal variant ST elevation in a young adult male
QoH NOT OMI HIGH CONFIDENCE
Case 22
This ECG is diagnostic of coronary occlusion. Inferior leads show very slight ST elevation and hyperacute T waves. (Most pronounced in lead III) Reciprocal changes in leads I and aVL. Inappropriately isoelectric ST segment in V2-V3. This is inferoposterior OMI.
QoH OMI HIGH CONFIDENCE.
Case 23
This ECG shows a ventricular rhythm @48bpm. This was not a reperfusion arrhythmia (they tend to be with a higher heart rate). There was no OMI. This patient has hypertrophic cardiomyopathy and is on beta blocker. When the sinus rate dropped into the 40s, a ventricular rhythm appeared with isorhythmic AV dissociation. ST segments are appropriately discordant.
QoH NOT OMI HIGH CONFINDENCE.
Case 24
This one now should be easy for you. No OMI here. Emery phenomenon mimicking a STEMI.
QoH NOT OMI HIGH CONFIDENCE
Case 25
This ECG shows a very subtle inferior wall MI. HATW inferior leads and T wave inversion in aVL. These changes were appreciated and the patient was referred for CAG that showed a totally occluded pRCA.
This was a false negative for the QoH. Version 2.0 will have four times as much training data. It is likely that the next version will diagnose this ECG.
Case 26
Is this inferoposterior OMI with STE in inferior leads, early R wave transition and reciprocal change in the lateral leads? No. This is another example of pseudoinfarct due to WpW pre-excitation.
QoH NOT OMI HIGH CONFIDENCE
Case 27
This ECG shows significant T wave changes. You might be tempted to call these hyperacute T waves. Look at the QTc, it is very prolonged as is often seen in stress cardiomyopathy. This ECG is consistent with Takotsubo cardiomyopathy. CT coronary angiogram was normal here. The patient was a young female without risk factors for CAD. This was a false positive for the Queen. Version 2.0 will have substantially more training data on Takotsubo and will hopefully and likely recognize this pattern as not OMI
RESULT
{number correct} out of 27
{percent correct} out of 100%
QoH version 1.0 got a percent correct of 89 (24/27)