What clinical scenario fits BEST?
This quiz consists of 10 different ECGs. Your task is to match the ECG with the clinical scenario / ECG description that you think fits BEST. You can choose from 5 different possible anwers for each case. All ECGs are 25mm/s.
NB! To enlarge images — Right-click for options on computers; Stretch image on tablet or smart phone. Good luck!
Created by Magnus Nossen

Which clinical scenario fits BEST with the ECG?
Which clinical scenario fits BEST with the ECG?
Which clinical scenario fits BEST with the ECG?
Which clinical scenario fits BEST with the ECG?
Which clinical scenario fits BEST with the ECG?
Which clinical scenario fits BEST with the ECG?
Which clinical scenario fits BEST with the ECG?

Which clinical scenario fits BEST with the ECG?
Which clinical scenario fits BEST with the ECG?

Which clinical scenario fits BEST with the ECG?
{number correct}/{number of questions} correct answers
Not impressive :( Go back to the books and try the Quiz again in one year.
Below are short explanations to ALL the cases.
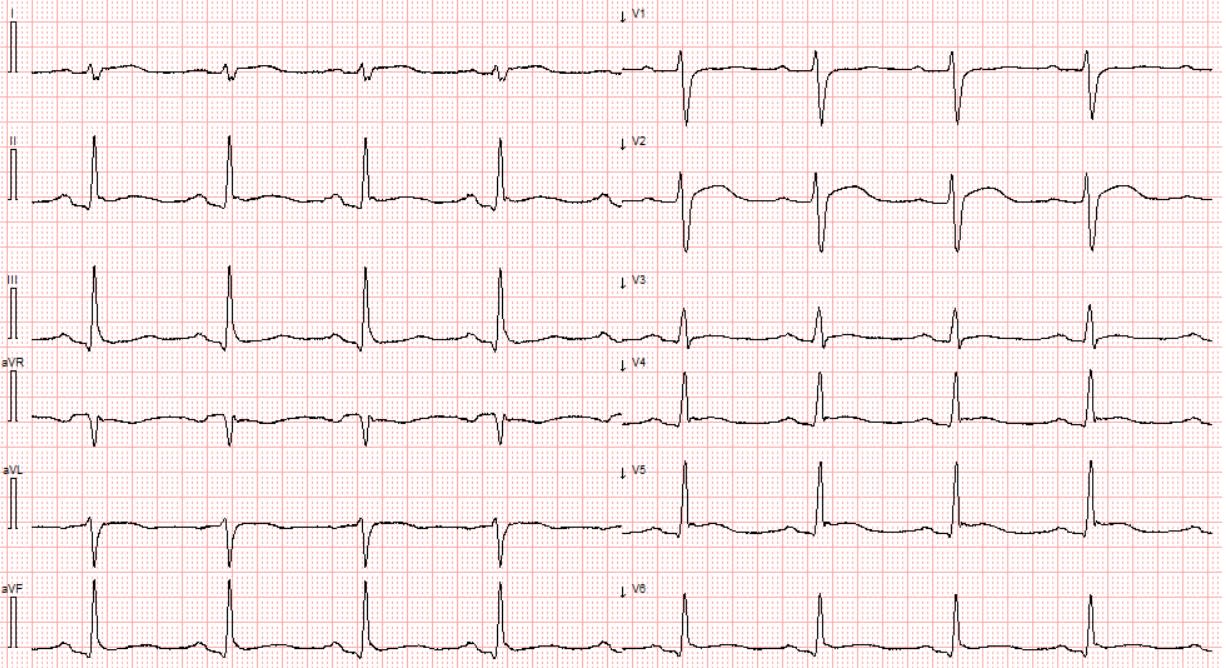
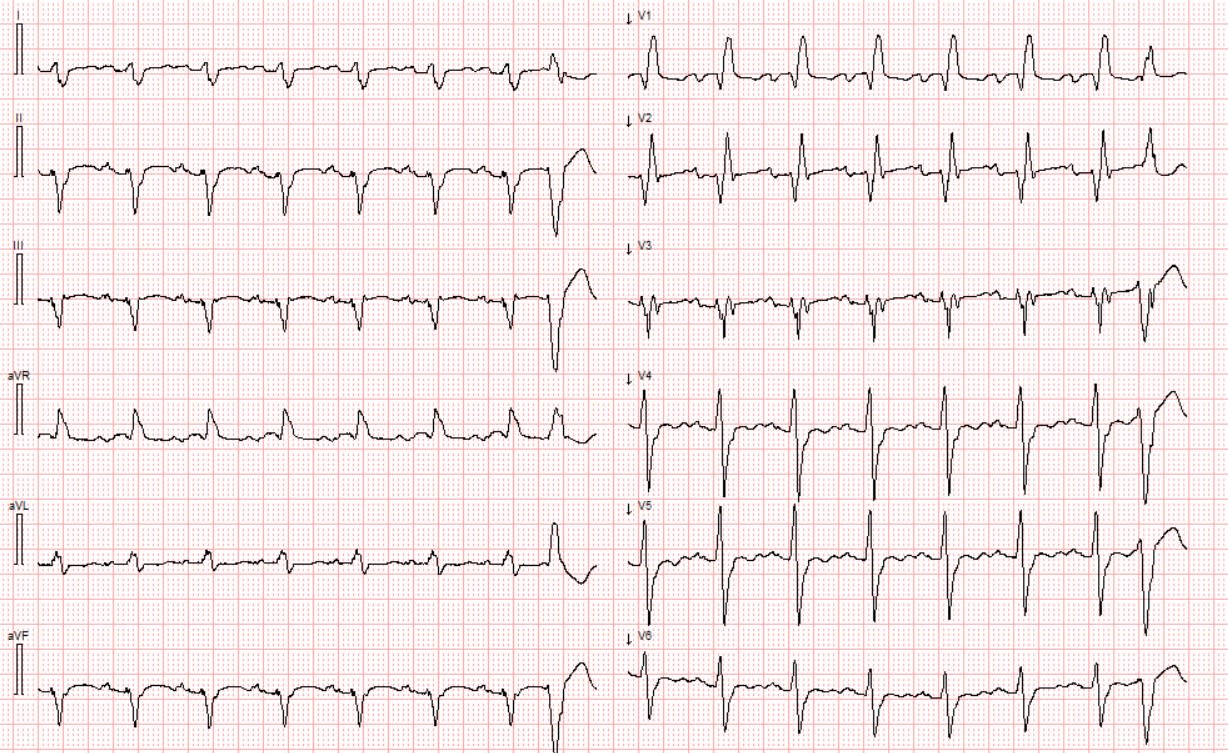
CASE #1 Clinical scenario: 17 year old with CP following a viral illness
SR, subtle STE in 9/12 leads w/o reciprocal STD. PR dep. R wave amplitude is preserved and no pathologic Q waves are visible. Findings c/w peri(myo)carditis. This patient developed massive STE. CT coronary angiography ruled out OMI. Myocarditis may be indistinguishable from OMI by ECG and may require cardiac cath to confirm the diagnosis and rule out OMI.
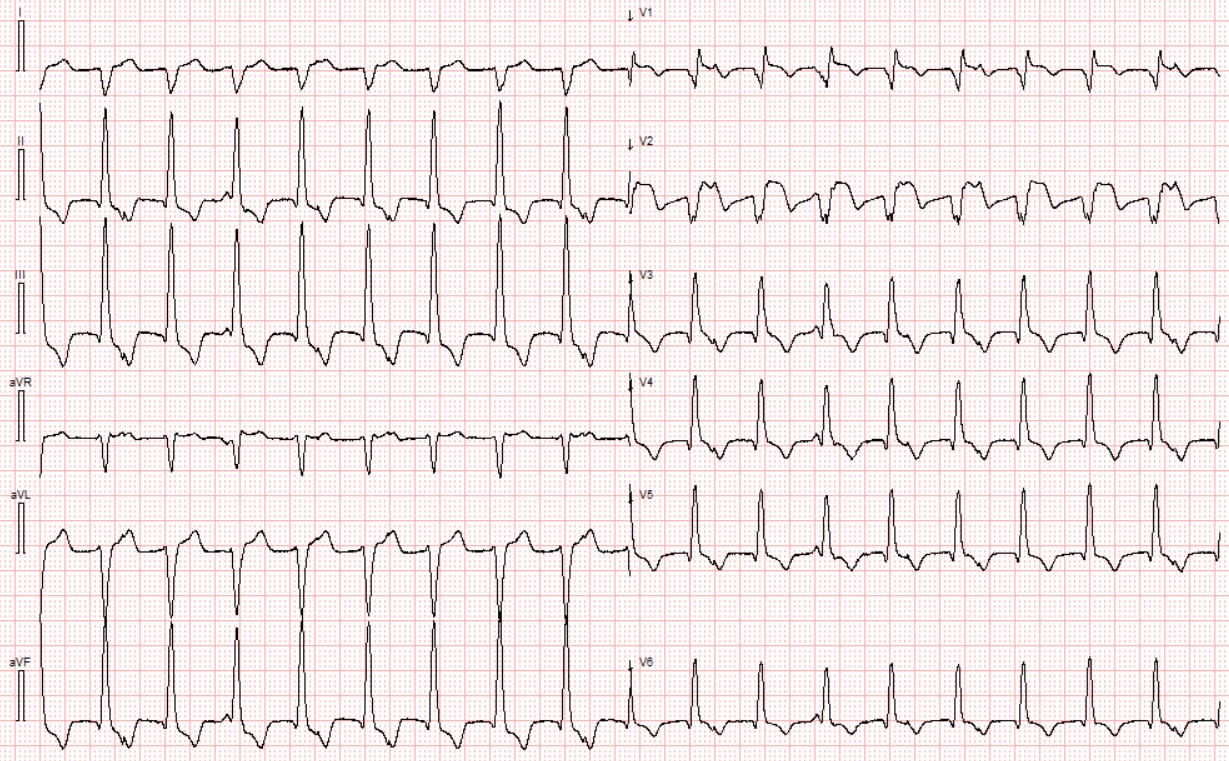
CASE #2 Clinical scenario: Tracing obtained after successful PCI of LAD.
A difficult tracing. Regular WCT at 115 bpm. Wide Q waves V1-V2 and abnormal appearing STE in these leads together with AV dissociation is consistent with an accelerated idioventricular rhythm (reperfusion rhythm) following PCI of the LAD. Prehospital ECG was c/w LAD OMI.
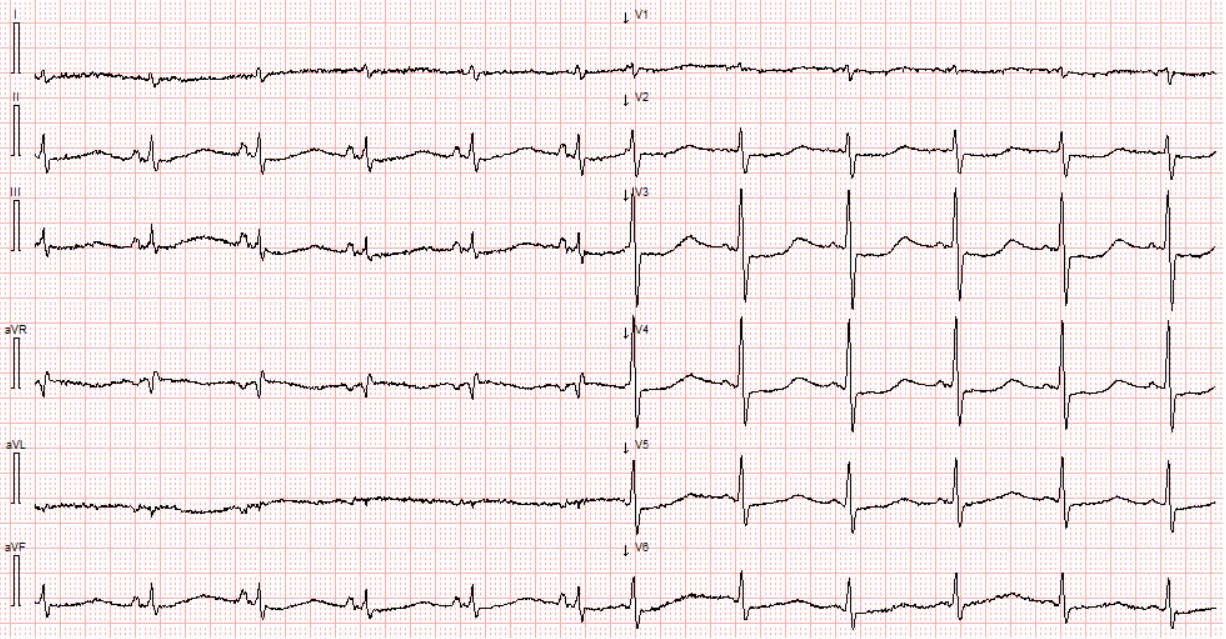
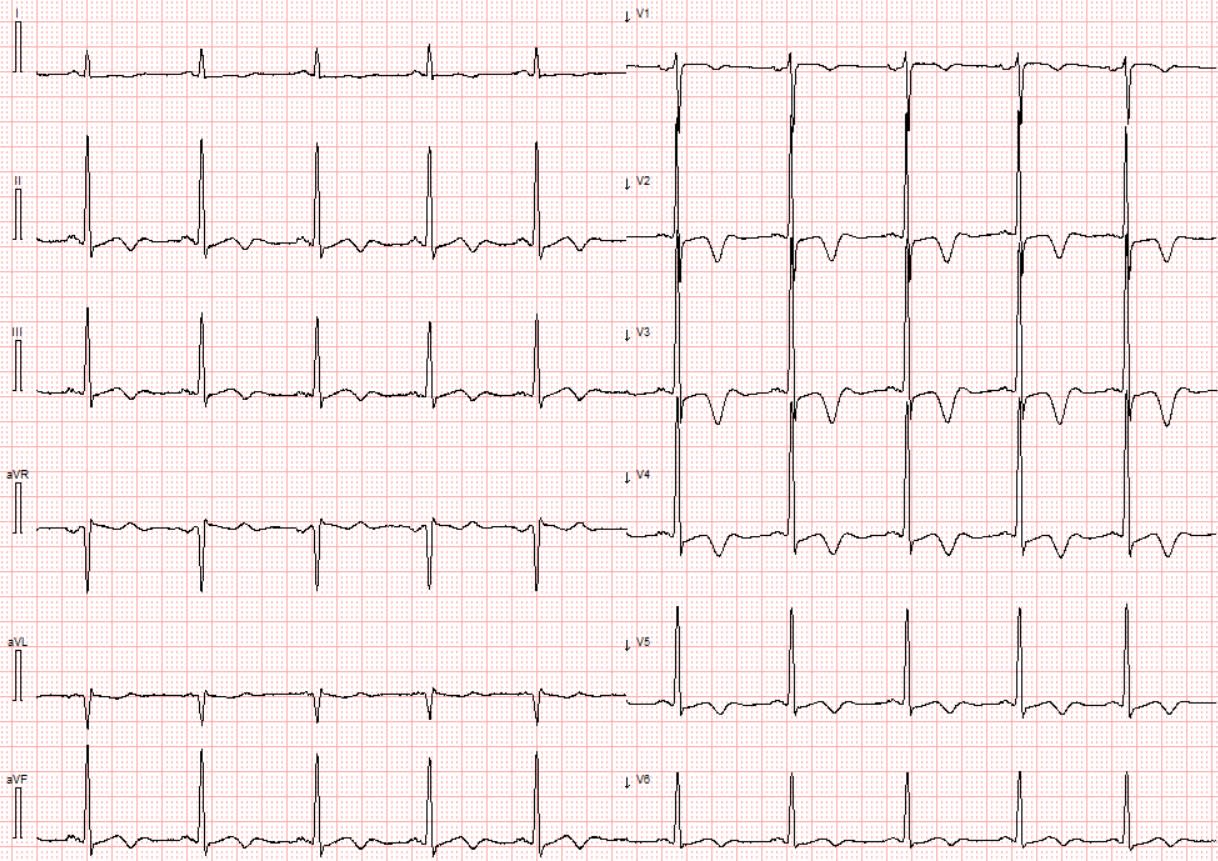
CASE #3 Clinical scenario: Multiple syncopal episodes after 7 days of "stomach flu"(press for ECG)
This ECG shows a very prolonged QTc interval with prominent U waves. This ECG is strongly suggest severe hypokalemia. Potassium was 1,4.
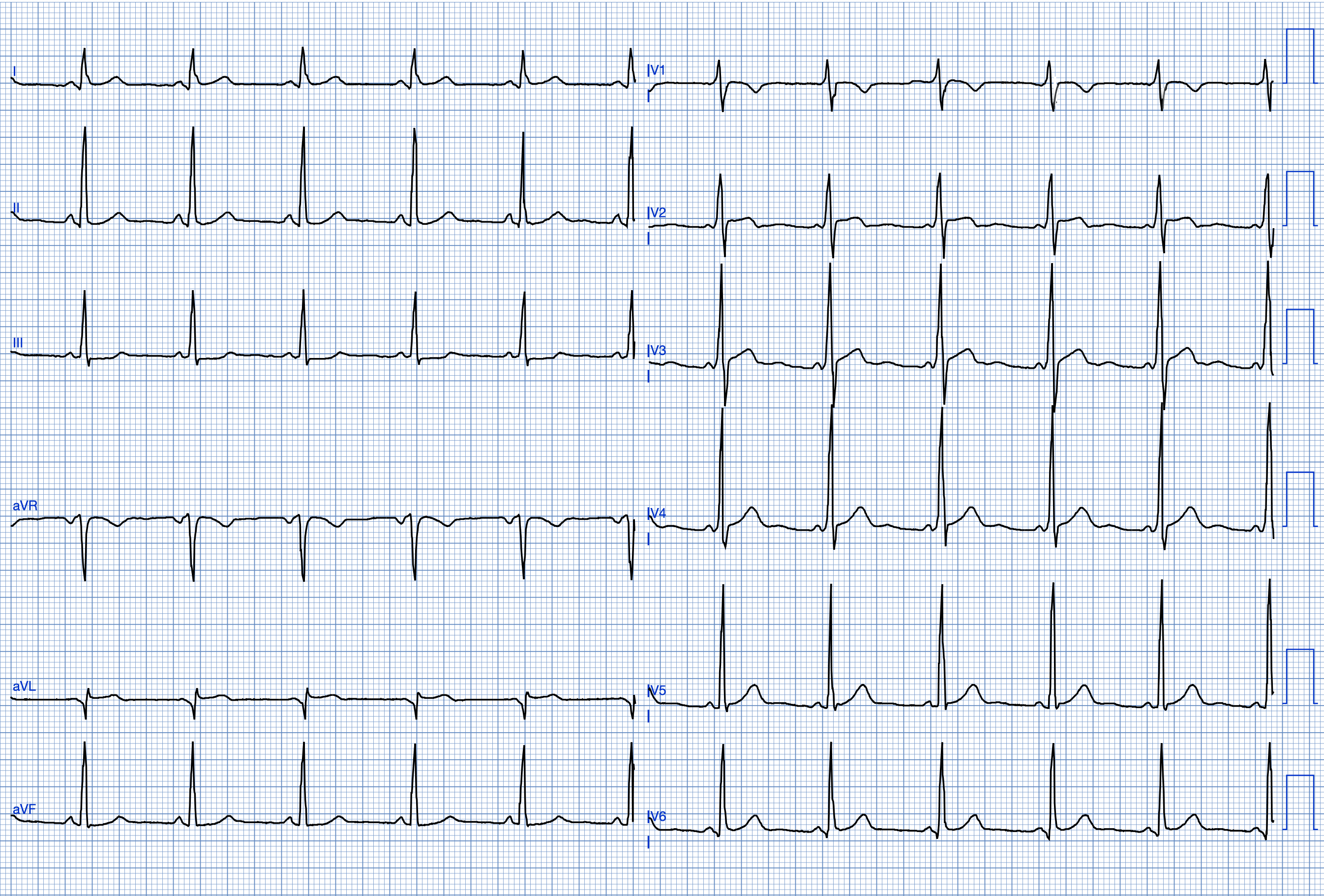
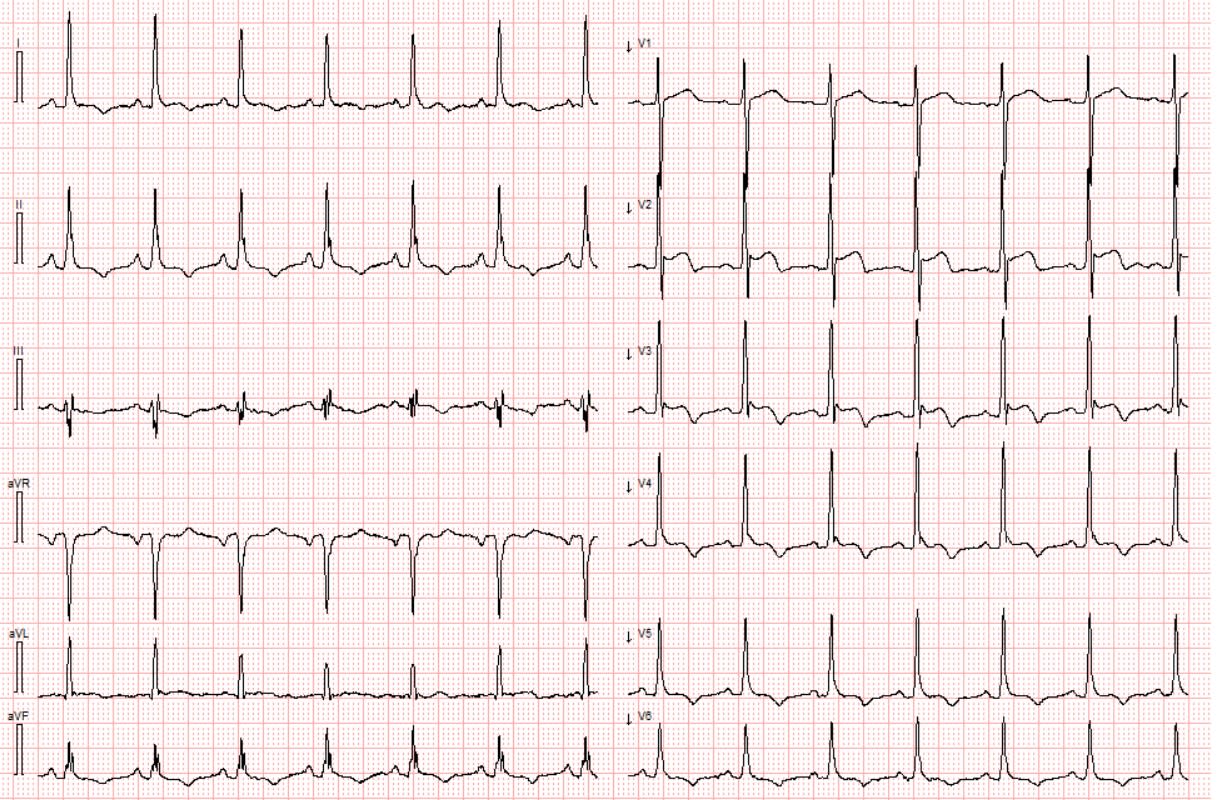
CASE #4 Clinical scenario: 29 year old male with "anxiety disorder"
SR with a very short PR interval, subtle delta waves in several leads and early R/S transition c/w preexcitation. When combined with a history consistent with arrhythmia this is Wolf-Parkinson-White syndrome. Not uncommonly, SVTs are misinterpreted as anxiety disorder if they terminate before an ECG can be obtained.
CASE #5 Clinical scenario: Dilated cardiomyopathy. EF 15%
Middle aged man with de novo heart failure. Diagnosed with dilated cardiomyopathy with severely reduced EF. The ECG shows bifascicular block and left atrial enlargement. Multi chamber enlargement and conduction blocks are common in dilated cardiomyopathy. Sinus tachycardia is a common finding with severely depressed EF. None of the other anwers are fully compatible with the ECG.
CASE #6 Clinical scenario: Asymptomatic patient with known Apical HCM
SR and large QRS voltages. Secondary repolarization abnormalities are present in the form of deep symmetric TWI in multiple leads which is typical of ApHCM.
CASE #7 clinical scenario: Baseline (old) ECG of patient who suffered V-fib arrest during sleep (press for ECG)
Type I Brugada morphology. This patient experienced V-fib arrest while sleeping. Brugada syndrome (BRS) and Early Repolarization Syndrome (ERS) constitute the J wave syndromes (JWS). JWS are clinically similar in their presentation. CA usually occurs during bradycardia and in situations characterized by increased vagal tone as occurs during sleep. Genetic testing revealed SCN5A mutation linked to BrS.
CASE #8 clinical scenario: Baseline ECG of an African American male
This ECG pattern may be confusing if you have not seen it before. If you have, it is instantly recognizable as benign T wave inversion (BTWI). Markedly increased voltage, distinct J waves with upward sloping STE and TWI in leads with STE. This ECG pattern is more commonly found in males of African heritage.
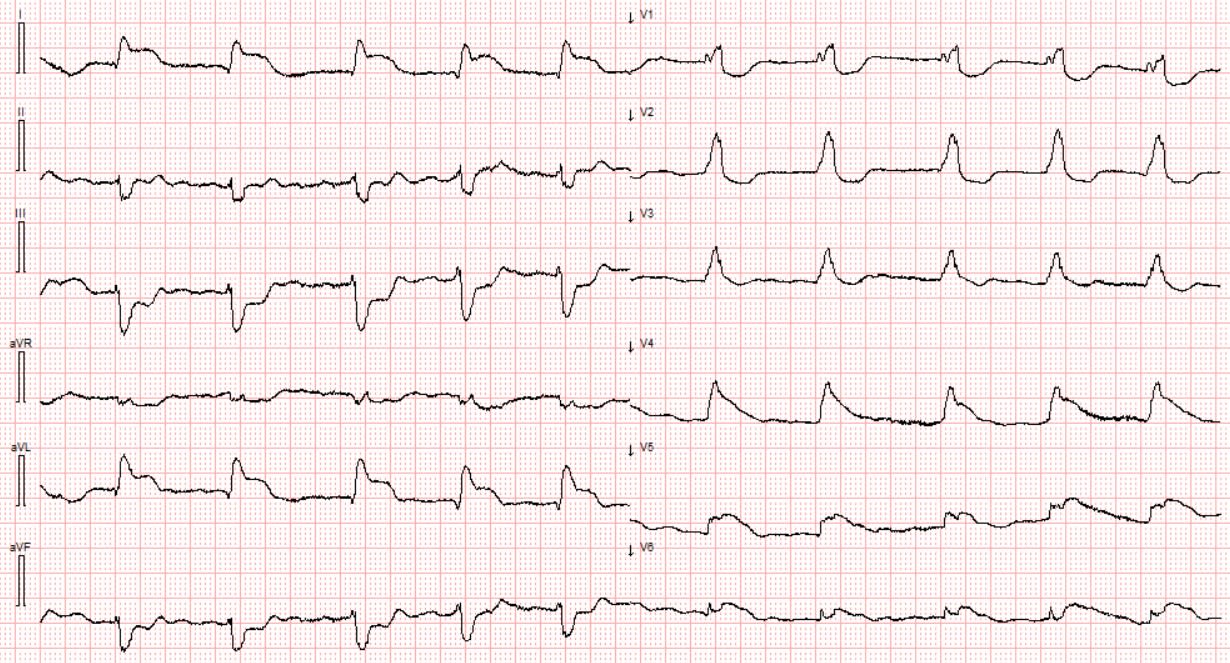
CASE #9 clinical scenario: Chest pain and RCA occlusion at cath
Very subtle STE and (possible) hyperacute T waves inferior leads. What makes this ECG diagnostic of OMI is the reciprocal change in aVL and ST flattening in V2-V3 that indicates associated posterior OMI. The patient was found to have a 100% occlusion of the pRCA.
CASE #10 clinical scenario: Obtunded, shocky with LMCA OMI at cath
ECG obtained from a 70 yo ill-appearing male. ECG shows afib with RBBB and LAFB. There is ST-segment elevation in leads V4-V6, I and aVL with several leads showing extensive ST depression. This patient arrested and received thrombolytics. He survived transport to the cath lab where LM was stented. LM is the best answer among the choices given. There is no "single" ECG picture for LM occlusion.
{number correct}/{number of questions} correct answers
Not impressive :( Go back to the books and try the Quiz again in one year.
Below are short explanations to ALL the cases.
CASE #1 Clinical scenario: 17 year old with CP following a viral illness
SR, subtle STE in 9/12 leads w/o reciprocal STD. PR dep. R wave amplitude is preserved and no pathologic Q waves are visible. Findings c/w peri(myo)carditis. This patient developed massive STE. CT coronary angiography ruled out OMI. Myocarditis may be indistinguishable from OMI by ECG and may require cardiac cath to confirm the diagnosis and rule out OMI.
CASE #2 Clinical scenario: Tracing obtained after successful PCI of LAD.
A difficult tracing. Regular WCT at 115 bpm. Wide Q waves V1-V2 and abnormal appearing STE in these leads together with AV dissociation is consistent with an accelerated idioventricular rhythm (reperfusion rhythm) following PCI of the LAD. Prehospital ECG was c/w LAD OMI.
CASE #3 Clinical scenario: Multiple syncopal episodes after 7 days of "stomach flu"(press for ECG)
This ECG shows a very prolonged QTc interval with prominent U waves. This ECG is strongly suggest severe hypokalemia. Potassium was 1,4.
CASE #4 Clinical scenario: 29 year old male with "anxiety disorder"
SR with a very short PR interval, subtle delta waves in several leads and early R/S transition c/w preexcitation. When combined with a history consistent with arrhythmia this is Wolf-Parkinson-White syndrome. Not uncommonly, SVTs are misinterpreted as anxiety disorder if they terminate before an ECG can be obtained.
CASE #5 Clinical scenario: Dilated cardiomyopathy. EF 15%
Middle aged man with de novo heart failure. Diagnosed with dilated cardiomyopathy with severely reduced EF. The ECG shows bifascicular block and left atrial enlargement. Multi chamber enlargement and conduction blocks are common in dilated cardiomyopathy. Sinus tachycardia is a common finding with severely depressed EF. None of the other anwers are fully compatible with the ECG.
CASE #6 Clinical scenario: Asymptomatic patient with known Apical HCM
SR and large QRS voltages. Secondary repolarization abnormalities are present in the form of deep symmetric TWI in multiple leads which is typical of ApHCM.
CASE #7 clinical scenario: Baseline (old) ECG of patient who suffered V-fib arrest during sleep (press for ECG)
Type I Brugada morphology. This patient experienced V-fib arrest while sleeping. Brugada syndrome (BRS) and Early Repolarization Syndrome (ERS) constitute the J wave syndromes (JWS). JWS are clinically similar in their presentation. CA usually occurs during bradycardia and in situations characterized by increased vagal tone as occurs during sleep. Genetic testing revealed SCN5A mutation linked to BrS.
CASE #8 clinical scenario: Baseline ECG of an African American male
This ECG pattern may be confusing if you have not seen it before. If you have, it is instantly recognizable as benign T wave inversion (BTWI). Markedly increased voltage, distinct J waves with upward sloping STE and TWI in leads with STE. This ECG pattern is more commonly found in males of African heritage.
CASE #9 clinical scenario: Chest pain and RCA occlusion at cath
Very subtle STE and (possible) hyperacute T waves inferior leads. What makes this ECG diagnostic of OMI is the reciprocal change in aVL and ST flattening in V2-V3 that indicates associated posterior OMI. The patient was found to have a 100% occlusion of the pRCA.
CASE #10 clinical scenario: Obtunded, shocky with LMCA OMI at cath
ECG obtained from a 70 yo ill-appearing male. ECG shows afib with RBBB and LAFB. There is ST-segment elevation in leads V4-V6, I and aVL with several leads showing extensive ST depression. This patient arrested and received thrombolytics. He survived transport to the cath lab where LM was stented. LM is the best answer among the choices given. There is no "single" ECG picture for LM occlusion.
{number correct}/{number of questions} correct answers
Decent try. Study hard and try the Quiz again in six months.
Below are short explanations to ALL the cases.
CASE #1 Clinical scenario: 17 year old with CP following a viral illness
SR, subtle STE in 9/12 leads w/o reciprocal STD. PR dep. R wave amplitude is preserved and no pathologic Q waves are visible. Findings c/w peri(myo)carditis. This patient developed massive STE. CT coronary angiography ruled out OMI. Myocarditis may be indistinguishable from OMI by ECG and may require cardiac cath to confirm the diagnosis and rule out OMI.
CASE #2 Clinical scenario: Tracing obtained after successful PCI of LAD.
A difficult tracing. Regular WCT at 115 bpm. Wide Q waves V1-V2 and abnormal appearing STE in these leads together with AV dissociation is consistent with an accelerated idioventricular rhythm (reperfusion rhythm) following PCI of the LAD. Prehospital ECG was c/w LAD OMI.
CASE #3 Clinical scenario: Multiple syncopal episodes after 7 days of "stomach flu"(press for ECG)
This ECG shows a very prolonged QTc interval with prominent U waves. This ECG is strongly suggest severe hypokalemia. Potassium was 1,4.
CASE #4 Clinical scenario: 29 year old male with "anxiety disorder"
SR with a very short PR interval, subtle delta waves in several leads and early R/S transition c/w preexcitation. When combined with a history consistent with arrhythmia this is Wolf-Parkinson-White syndrome. Not uncommonly, SVTs are misinterpreted as anxiety disorder if they terminate before an ECG can be obtained.
CASE #5 Clinical scenario: Dilated cardiomyopathy. EF 15%
Middle aged man with de novo heart failure. Diagnosed with dilated cardiomyopathy with severely reduced EF. The ECG shows bifascicular block and left atrial enlargement. Multi chamber enlargement and conduction blocks are common in dilated cardiomyopathy. Sinus tachycardia is a common finding with severely depressed EF. None of the other anwers are fully compatible with the ECG.
CASE #6 Clinical scenario: Asymptomatic patient with known Apical HCM
SR and large QRS voltages. Secondary repolarization abnormalities are present in the form of deep symmetric TWI in multiple leads which is typical of ApHCM.
CASE #7 clinical scenario: Baseline (old) ECG of patient who suffered V-fib arrest during sleep (press for ECG)
Type I Brugada morphology. This patient experienced V-fib arrest while sleeping. Brugada syndrome (BRS) and Early Repolarization Syndrome (ERS) constitute the J wave syndromes (JWS). JWS are clinically similar in their presentation. CA usually occurs during bradycardia and in situations characterized by increased vagal tone as occurs during sleep. Genetic testing revealed SCN5A mutation linked to BrS.
CASE #8 clinical scenario: Baseline ECG of an African American male
This ECG pattern may be confusing if you have not seen it before. If you have, it is instantly recognizable as benign T wave inversion (BTWI). Markedly increased voltage, distinct J waves with upward sloping STE and TWI in leads with STE. This ECG pattern is more commonly found in males of African heritage.
CASE #9 clinical scenario: Chest pain and RCA occlusion at cath
Very subtle STE and (possible) hyperacute T waves inferior leads. What makes this ECG diagnostic of OMI is the reciprocal change in aVL and ST flattening in V2-V3 that indicates associated posterior OMI. The patient was found to have a 100% occlusion of the pRCA.
CASE #10 clinical scenario: Obtunded, shocky with LMCA OMI at cath
ECG obtained from a 70 yo ill-appearing male. ECG shows afib with RBBB and LAFB. There is ST-segment elevation in leads V4-V6, I and aVL with several leads showing extensive ST depression. This patient arrested and received thrombolytics. He survived transport to the cath lab where LM was stented. LM is the best answer among the choices given. There is no "single" ECG picture for LM occlusion.
{number correct}/{number of questions} correct answers
Decent try. Study hard and try the Quiz again in six months.
Below are short explanations to ALL the cases.
CASE #1 Clinical scenario: 17 year old with CP following a viral illness
SR, subtle STE in 9/12 leads w/o reciprocal STD. PR dep. R wave amplitude is preserved and no pathologic Q waves are visible. Findings c/w peri(myo)carditis. This patient developed massive STE. CT coronary angiography ruled out OMI. Myocarditis may be indistinguishable from OMI by ECG and may require cardiac cath to confirm the diagnosis and rule out OMI.
CASE #2 Clinical scenario: Tracing obtained after successful PCI of LAD.
A difficult tracing. Regular WCT at 115 bpm. Wide Q waves V1-V2 and abnormal appearing STE in these leads together with AV dissociation is consistent with an accelerated idioventricular rhythm (reperfusion rhythm) following PCI of the LAD. Prehospital ECG was c/w LAD OMI.
CASE #3 Clinical scenario: Multiple syncopal episodes after 7 days of "stomach flu"(press for ECG)
This ECG shows a very prolonged QTc interval with prominent U waves. This ECG is strongly suggest severe hypokalemia. Potassium was 1,4.
CASE #4 Clinical scenario: 29 year old male with "anxiety disorder"
SR with a very short PR interval, subtle delta waves in several leads and early R/S transition c/w preexcitation. When combined with a history consistent with arrhythmia this is Wolf-Parkinson-White syndrome. Not uncommonly, SVTs are misinterpreted as anxiety disorder if they terminate before an ECG can be obtained.
CASE #5 Clinical scenario: Dilated cardiomyopathy. EF 15%
Middle aged man with de novo heart failure. Diagnosed with dilated cardiomyopathy with severely reduced EF. The ECG shows bifascicular block and left atrial enlargement. Multi chamber enlargement and conduction blocks are common in dilated cardiomyopathy. Sinus tachycardia is a common finding with severely depressed EF. None of the other anwers are fully compatible with the ECG.
CASE #6 Clinical scenario: Asymptomatic patient with known Apical HCM
SR and large QRS voltages. Secondary repolarization abnormalities are present in the form of deep symmetric TWI in multiple leads which is typical of ApHCM.
CASE #7 clinical scenario: Baseline (old) ECG of patient who suffered V-fib arrest during sleep (press for ECG)
Type I Brugada morphology. This patient experienced V-fib arrest while sleeping. Brugada syndrome (BRS) and Early Repolarization Syndrome (ERS) constitute the J wave syndromes (JWS). JWS are clinically similar in their presentation. CA usually occurs during bradycardia and in situations characterized by increased vagal tone as occurs during sleep. Genetic testing revealed SCN5A mutation linked to BrS.
CASE #8 clinical scenario: Baseline ECG of an African American male
This ECG pattern may be confusing if you have not seen it before. If you have, it is instantly recognizable as benign T wave inversion (BTWI). Markedly increased voltage, distinct J waves with upward sloping STE and TWI in leads with STE. This ECG pattern is more commonly found in males of African heritage.
CASE #9 clinical scenario: Chest pain and RCA occlusion at cath
Very subtle STE and (possible) hyperacute T waves inferior leads. What makes this ECG diagnostic of OMI is the reciprocal change in aVL and ST flattening in V2-V3 that indicates associated posterior OMI. The patient was found to have a 100% occlusion of the pRCA.
CASE #10 clinical scenario: Obtunded, shocky with LMCA OMI at cath
ECG obtained from a 70 yo ill-appearing male. ECG shows afib with RBBB and LAFB. There is ST-segment elevation in leads V4-V6, I and aVL with several leads showing extensive ST depression. This patient arrested and received thrombolytics. He survived transport to the cath lab where LM was stented. LM is the best answer among the choices given. There is no "single" ECG picture for LM occlusion.
{number correct}/{number of questions} correct answers
Not too bad! Read the answes to see if you can learn something.
Below are short explanations to ALL the cases.
CASE #1 Clinical scenario: 17 year old with CP following a viral illness
SR, subtle STE in 9/12 leads w/o reciprocal STD. PR dep. R wave amplitude is preserved and no pathologic Q waves are visible. Findings c/w peri(myo)carditis. This patient developed massive STE. CT coronary angiography ruled out OMI. Myocarditis may be indistinguishable from OMI by ECG and may require cardiac cath to confirm the diagnosis and rule out OMI.
CASE #2 Clinical scenario: Tracing obtained after successful PCI of LAD.
A difficult tracing. Regular WCT at 115 bpm. Wide Q waves V1-V2 and abnormal appearing STE in these leads together with AV dissociation is consistent with an accelerated idioventricular rhythm (reperfusion rhythm) following PCI of the LAD. Prehospital ECG was c/w LAD OMI.
CASE #3 Clinical scenario: Multiple syncopal episodes after 7 days of "stomach flu"(press for ECG)
This ECG shows a very prolonged QTc interval with prominent U waves. This ECG is strongly suggest severe hypokalemia. Potassium was 1,4.
CASE #4 Clinical scenario: 29 year old male with "anxiety disorder"
SR with a very short PR interval, subtle delta waves in several leads and early R/S transition c/w preexcitation. When combined with a history consistent with arrhythmia this is Wolf-Parkinson-White syndrome. Not uncommonly, SVTs are misinterpreted as anxiety disorder if they terminate before an ECG can be obtained.
CASE #5 Clinical scenario: Dilated cardiomyopathy. EF 15%
Middle aged man with de novo heart failure. Diagnosed with dilated cardiomyopathy with severely reduced EF. The ECG shows bifascicular block and left atrial enlargement. Multi chamber enlargement and conduction blocks are common in dilated cardiomyopathy. Sinus tachycardia is a common finding with severely depressed EF. None of the other anwers are fully compatible with the ECG.
CASE #6 Clinical scenario: Asymptomatic patient with known Apical HCM
SR and large QRS voltages. Secondary repolarization abnormalities are present in the form of deep symmetric TWI in multiple leads which is typical of ApHCM.
CASE #7 clinical scenario: Baseline (old) ECG of patient who suffered V-fib arrest during sleep (press for ECG)
Type I Brugada morphology. This patient experienced V-fib arrest while sleeping. Brugada syndrome (BRS) and Early Repolarization Syndrome (ERS) constitute the J wave syndromes (JWS). JWS are clinically similar in their presentation. CA usually occurs during bradycardia and in situations characterized by increased vagal tone as occurs during sleep. Genetic testing revealed SCN5A mutation linked to BrS.
CASE #8 clinical scenario: Baseline ECG of an African American male
This ECG pattern may be confusing if you have not seen it before. If you have, it is instantly recognizable as benign T wave inversion (BTWI). Markedly increased voltage, distinct J waves with upward sloping STE and TWI in leads with STE. This ECG pattern is more commonly found in males of African heritage.
CASE #9 clinical scenario: Chest pain and RCA occlusion at cath
Very subtle STE and (possible) hyperacute T waves inferior leads. What makes this ECG diagnostic of OMI is the reciprocal change in aVL and ST flattening in V2-V3 that indicates associated posterior OMI. The patient was found to have a 100% occlusion of the pRCA.
CASE #10 clinical scenario: Obtunded, shocky with LMCA OMI at cath
ECG obtained from a 70 yo ill-appearing male. ECG shows afib with RBBB and LAFB. There is ST-segment elevation in leads V4-V6, I and aVL with several leads showing extensive ST depression. This patient arrested and received thrombolytics. He survived transport to the cath lab where LM was stented. LM is the best answer among the choices given. There is no "single" ECG picture for LM occlusion.
{number correct}/{number of questions} correct answers
Good work! You know your stuff! Keep styding ECGs and you'll become an expert!
Below are short explanations to ALL the cases.
CASE #1 Clinical scenario: 17 year old with CP following a viral illness
SR, subtle STE in 9/12 leads w/o reciprocal STD. PR dep. R wave amplitude is preserved and no pathologic Q waves are visible. Findings c/w peri(myo)carditis. This patient developed massive STE. CT coronary angiography ruled out OMI. Myocarditis may be indistinguishable from OMI by ECG and may require cardiac cath to confirm the diagnosis and rule out OMI.
CASE #2 Clinical scenario: Tracing obtained after successful PCI of LAD.
A difficult tracing. Regular WCT at 115 bpm. Wide Q waves V1-V2 and abnormal appearing STE in these leads together with AV dissociation is consistent with an accelerated idioventricular rhythm (reperfusion rhythm) following PCI of the LAD. Prehospital ECG was c/w LAD OMI.
CASE #3 Clinical scenario: Multiple syncopal episodes after 7 days of "stomach flu"(press for ECG)
This ECG shows a very prolonged QTc interval with prominent U waves. This ECG is strongly suggest severe hypokalemia. Potassium was 1,4.
CASE #4 Clinical scenario: 29 year old male with "anxiety disorder"
SR with a very short PR interval, subtle delta waves in several leads and early R/S transition c/w preexcitation. When combined with a history consistent with arrhythmia this is Wolf-Parkinson-White syndrome. Not uncommonly, SVTs are misinterpreted as anxiety disorder if they terminate before an ECG can be obtained.
CASE #5 Clinical scenario: Dilated cardiomyopathy. EF 15%
Middle aged man with de novo heart failure. Diagnosed with dilated cardiomyopathy with severely reduced EF. The ECG shows bifascicular block and left atrial enlargement. Multi chamber enlargement and conduction blocks are common in dilated cardiomyopathy. Sinus tachycardia is a common finding with severely depressed EF. None of the other anwers are fully compatible with the ECG.
CASE #6 Clinical scenario: Asymptomatic patient with known Apical HCM
SR and large QRS voltages. Secondary repolarization abnormalities are present in the form of deep symmetric TWI in multiple leads which is typical of ApHCM.
CASE #7 clinical scenario: Baseline (old) ECG of patient who suffered V-fib arrest during sleep (press for ECG)
Type I Brugada morphology. This patient experienced V-fib arrest while sleeping. Brugada syndrome (BRS) and Early Repolarization Syndrome (ERS) constitute the J wave syndromes (JWS). JWS are clinically similar in their presentation. CA usually occurs during bradycardia and in situations characterized by increased vagal tone as occurs during sleep. Genetic testing revealed SCN5A mutation linked to BrS.
CASE #8 clinical scenario: Baseline ECG of an African American male
This ECG pattern may be confusing if you have not seen it before. If you have, it is instantly recognizable as benign T wave inversion (BTWI). Markedly increased voltage, distinct J waves with upward sloping STE and TWI in leads with STE. This ECG pattern is more commonly found in males of African heritage.
CASE #9 clinical scenario: Chest pain and RCA occlusion at cath
Very subtle STE and (possible) hyperacute T waves inferior leads. What makes this ECG diagnostic of OMI is the reciprocal change in aVL and ST flattening in V2-V3 that indicates associated posterior OMI. The patient was found to have a 100% occlusion of the pRCA.
CASE #10 clinical scenario: Obtunded, shocky with LMCA OMI at cath
ECG obtained from a 70 yo ill-appearing male. ECG shows afib with RBBB and LAFB. There is ST-segment elevation in leads V4-V6, I and aVL with several leads showing extensive ST depression. This patient arrested and received thrombolytics. He survived transport to the cath lab where LM was stented. LM is the best answer among the choices given. There is no "single" ECG picture for LM occlusion.
{number correct}/{number of questions} correct answers
Great job! 7/10 is really good on this Quiz!
Below are short explanations to ALL the cases.
CASE #1 Clinical scenario: 17 year old with CP following a viral illness
SR, subtle STE in 9/12 leads w/o reciprocal STD. PR dep. R wave amplitude is preserved and no pathologic Q waves are visible. Findings c/w peri(myo)carditis. This patient developed massive STE. CT coronary angiography ruled out OMI. Myocarditis may be indistinguishable from OMI by ECG and may require cardiac cath to confirm the diagnosis and rule out OMI.
CASE #2 Clinical scenario: Tracing obtained after successful PCI of LAD.
A difficult tracing. Regular WCT at 115 bpm. Wide Q waves V1-V2 and abnormal appearing STE in these leads together with AV dissociation is consistent with an accelerated idioventricular rhythm (reperfusion rhythm) following PCI of the LAD. Prehospital ECG was c/w LAD OMI.
CASE #3 Clinical scenario: Multiple syncopal episodes after 7 days of "stomach flu"(press for ECG)
This ECG shows a very prolonged QTc interval with prominent U waves. This ECG is strongly suggest severe hypokalemia. Potassium was 1,4.
CASE #4 Clinical scenario: 29 year old male with "anxiety disorder"
SR with a very short PR interval, subtle delta waves in several leads and early R/S transition c/w preexcitation. When combined with a history consistent with arrhythmia this is Wolf-Parkinson-White syndrome. Not uncommonly, SVTs are misinterpreted as anxiety disorder if they terminate before an ECG can be obtained.
CASE #5 Clinical scenario: Dilated cardiomyopathy. EF 15%
Middle aged man with de novo heart failure. Diagnosed with dilated cardiomyopathy with severely reduced EF. The ECG shows bifascicular block and left atrial enlargement. Multi chamber enlargement and conduction blocks are common in dilated cardiomyopathy. Sinus tachycardia is a common finding with severely depressed EF. None of the other anwers are fully compatible with the ECG.
CASE #6 Clinical scenario: Asymptomatic patient with known Apical HCM
SR and large QRS voltages. Secondary repolarization abnormalities are present in the form of deep symmetric TWI in multiple leads which is typical of ApHCM.
CASE #7 clinical scenario: Baseline (old) ECG of patient who suffered V-fib arrest during sleep (press for ECG)
Type I Brugada morphology. This patient experienced V-fib arrest while sleeping. Brugada syndrome (BRS) and Early Repolarization Syndrome (ERS) constitute the J wave syndromes (JWS). JWS are clinically similar in their presentation. CA usually occurs during bradycardia and in situations characterized by increased vagal tone as occurs during sleep. Genetic testing revealed SCN5A mutation linked to BrS.
CASE #8 clinical scenario: Baseline ECG of an African American male
This ECG pattern may be confusing if you have not seen it before. If you have, it is instantly recognizable as benign T wave inversion (BTWI). Markedly increased voltage, distinct J waves with upward sloping STE and TWI in leads with STE. This ECG pattern is more commonly found in males of African heritage.
CASE #9 clinical scenario: Chest pain and RCA occlusion at cath
Very subtle STE and (possible) hyperacute T waves inferior leads. What makes this ECG diagnostic of OMI is the reciprocal change in aVL and ST flattening in V2-V3 that indicates associated posterior OMI. The patient was found to have a 100% occlusion of the pRCA.
CASE #10 clinical scenario: Obtunded, shocky with LMCA OMI at cath
ECG obtained from a 70 yo ill-appearing male. ECG shows afib with RBBB and LAFB. There is ST-segment elevation in leads V4-V6, I and aVL with several leads showing extensive ST depression. This patient arrested and received thrombolytics. He survived transport to the cath lab where LM was stented. LM is the best answer among the choices given. There is no "single" ECG picture for LM occlusion.
{number correct}/{number of questions} correct answers
Nice job!!! You are probably teaching ECGs! If not you should!
Below are short explanations to ALL the cases.
CASE #1 Clinical scenario: 17 year old with CP following a viral illness
SR, subtle STE in 9/12 leads w/o reciprocal STD. PR dep. R wave amplitude is preserved and no pathologic Q waves are visible. Findings c/w peri(myo)carditis. This patient developed massive STE. CT coronary angiography ruled out OMI. Myocarditis may be indistinguishable from OMI by ECG and may require cardiac cath to confirm the diagnosis and rule out OMI.
CASE #2 Clinical scenario: Tracing obtained after successful PCI of LAD.
A difficult tracing. Regular WCT at 115 bpm. Wide Q waves V1-V2 and abnormal appearing STE in these leads together with AV dissociation is consistent with an accelerated idioventricular rhythm (reperfusion rhythm) following PCI of the LAD. Prehospital ECG was c/w LAD OMI.
CASE #3 Clinical scenario: Multiple syncopal episodes after 7 days of "stomach flu"(press for ECG)
This ECG shows a very prolonged QTc interval with prominent U waves. This ECG is strongly suggest severe hypokalemia. Potassium was 1,4.
CASE #4 Clinical scenario: 29 year old male with "anxiety disorder"
SR with a very short PR interval, subtle delta waves in several leads and early R/S transition c/w preexcitation. When combined with a history consistent with arrhythmia this is Wolf-Parkinson-White syndrome. Not uncommonly, SVTs are misinterpreted as anxiety disorder if they terminate before an ECG can be obtained.
CASE #5 Clinical scenario: Dilated cardiomyopathy. EF 15%
Middle aged man with de novo heart failure. Diagnosed with dilated cardiomyopathy with severely reduced EF. The ECG shows bifascicular block and left atrial enlargement. Multi chamber enlargement and conduction blocks are common in dilated cardiomyopathy. Sinus tachycardia is a common finding with severely depressed EF. None of the other anwers are fully compatible with the ECG.
CASE #6 Clinical scenario: Asymptomatic patient with known Apical HCM
SR and large QRS voltages. Secondary repolarization abnormalities are present in the form of deep symmetric TWI in multiple leads which is typical of ApHCM.
CASE #7 clinical scenario: Baseline (old) ECG of patient who suffered V-fib arrest during sleep (press for ECG)
Type I Brugada morphology. This patient experienced V-fib arrest while sleeping. Brugada syndrome (BRS) and Early Repolarization Syndrome (ERS) constitute the J wave syndromes (JWS). JWS are clinically similar in their presentation. CA usually occurs during bradycardia and in situations characterized by increased vagal tone as occurs during sleep. Genetic testing revealed SCN5A mutation linked to BrS.
CASE #8 clinical scenario: Baseline ECG of an African American male
This ECG pattern may be confusing if you have not seen it before. If you have, it is instantly recognizable as benign T wave inversion (BTWI). Markedly increased voltage, distinct J waves with upward sloping STE and TWI in leads with STE. This ECG pattern is more commonly found in males of African heritage.
CASE #9 clinical scenario: Chest pain and RCA occlusion at cath
Very subtle STE and (possible) hyperacute T waves inferior leads. What makes this ECG diagnostic of OMI is the reciprocal change in aVL and ST flattening in V2-V3 that indicates associated posterior OMI. The patient was found to have a 100% occlusion of the pRCA.
CASE #10 clinical scenario: Obtunded, shocky with LMCA OMI at cath
ECG obtained from a 70 yo ill-appearing male. ECG shows afib with RBBB and LAFB. There is ST-segment elevation in leads V4-V6, I and aVL with several leads showing extensive ST depression. This patient arrested and received thrombolytics. He survived transport to the cath lab where LM was stented. LM is the best answer among the choices given. There is no "single" ECG picture for LM occlusion.
{number correct}/{number of questions} correct answers
Outstanding! You are likely an experienced clinician and ECG enthusiast!
Below are short explanations to ALL the cases.
CASE #1 Clinical scenario: 17 year old with CP following a viral illness
SR, subtle STE in 9/12 leads w/o reciprocal STD. PR dep. R wave amplitude is preserved and no pathologic Q waves are visible. Findings c/w peri(myo)carditis. This patient developed massive STE. CT coronary angiography ruled out OMI. Myocarditis may be indistinguishable from OMI by ECG and may require cardiac cath to confirm the diagnosis and rule out OMI.
CASE #2 Clinical scenario: Tracing obtained after successful PCI of LAD.
A difficult tracing. Regular WCT at 115 bpm. Wide Q waves V1-V2 and abnormal appearing STE in these leads together with AV dissociation is consistent with an accelerated idioventricular rhythm (reperfusion rhythm) following PCI of the LAD. Prehospital ECG was c/w LAD OMI.
CASE #3 Clinical scenario: Multiple syncopal episodes after 7 days of "stomach flu"(press for ECG)
This ECG shows a very prolonged QTc interval with prominent U waves. This ECG is strongly suggest severe hypokalemia. Potassium was 1,4.
CASE #4 Clinical scenario: 29 year old male with "anxiety disorder"
SR with a very short PR interval, subtle delta waves in several leads and early R/S transition c/w preexcitation. When combined with a history consistent with arrhythmia this is Wolf-Parkinson-White syndrome. Not uncommonly, SVTs are misinterpreted as anxiety disorder if they terminate before an ECG can be obtained.
CASE #5 Clinical scenario: Dilated cardiomyopathy. EF 15%
Middle aged man with de novo heart failure. Diagnosed with dilated cardiomyopathy with severely reduced EF. The ECG shows bifascicular block and left atrial enlargement. Multi chamber enlargement and conduction blocks are common in dilated cardiomyopathy. Sinus tachycardia is a common finding with severely depressed EF. None of the other anwers are fully compatible with the ECG.
CASE #6 Clinical scenario: Asymptomatic patient with known Apical HCM
SR and large QRS voltages. Secondary repolarization abnormalities are present in the form of deep symmetric TWI in multiple leads which is typical of ApHCM.
CASE #7 clinical scenario: Baseline (old) ECG of patient who suffered V-fib arrest during sleep (press for ECG)
Type I Brugada morphology. This patient experienced V-fib arrest while sleeping. Brugada syndrome (BRS) and Early Repolarization Syndrome (ERS) constitute the J wave syndromes (JWS). JWS are clinically similar in their presentation. CA usually occurs during bradycardia and in situations characterized by increased vagal tone as occurs during sleep. Genetic testing revealed SCN5A mutation linked to BrS.
CASE #8 clinical scenario: Baseline ECG of an African American male
This ECG pattern may be confusing if you have not seen it before. If you have, it is instantly recognizable as benign T wave inversion (BTWI). Markedly increased voltage, distinct J waves with upward sloping STE and TWI in leads with STE. This ECG pattern is more commonly found in males of African heritage.
CASE #9 clinical scenario: Chest pain and RCA occlusion at cath
Very subtle STE and (possible) hyperacute T waves inferior leads. What makes this ECG diagnostic of OMI is the reciprocal change in aVL and ST flattening in V2-V3 that indicates associated posterior OMI. The patient was found to have a 100% occlusion of the pRCA.
CASE #10 clinical scenario: Obtunded, shocky with LMCA OMI at cath
ECG obtained from a 70 yo ill-appearing male. ECG shows afib with RBBB and LAFB. There is ST-segment elevation in leads V4-V6, I and aVL with several leads showing extensive ST depression. This patient arrested and received thrombolytics. He survived transport to the cath lab where LM was stented. LM is the best answer among the choices given. There is no "single" ECG picture for LM occlusion.
{number correct}{number of questions} correct answers
A PERFECT score! You probably have an unhealthy relationship with ECGs and should spend more time not studying squiggly lines.
CASE #1 Clinical scenario: 17 year old with CP following a viral illness
SR, subtle STE in 9/12 leads w/o reciprocal STD. PR dep. R wave amplitude is preserved and no pathologic Q waves are visible. Findings c/w peri(myo)carditis. This patient developed massive STE. CT coronary angiography ruled out OMI. Myocarditis may be indistinguishable from OMI by ECG and may require cardiac cath to confirm the diagnosis and rule out OMI.
CASE #2 Clinical scenario: Tracing obtained after successful PCI of LAD.
A difficult tracing. Regular WCT at 115 bpm. Wide Q waves V1-V2 and abnormal appearing STE in these leads together with AV dissociation is consistent with an accelerated idioventricular rhythm (reperfusion rhythm) following PCI of the LAD. Prehospital ECG was c/w LAD OMI.
CASE #3 Clinical scenario: Multiple syncopal episodes after 7 days of "stomach flu"(press for ECG)
This ECG shows a very prolonged QTc interval with prominent U waves. This ECG is strongly suggest severe hypokalemia. Potassium was 1,4.
CASE #4 Clinical scenario: 29 year old male with "anxiety disorder"
SR with a very short PR interval, subtle delta waves in several leads and early R/S transition c/w preexcitation. When combined with a history consistent with arrhythmia this is Wolf-Parkinson-White syndrome. Not uncommonly, SVTs are misinterpreted as anxiety disorder if they terminate before an ECG can be obtained.
CASE #5 Clinical scenario: Dilated cardiomyopathy. EF 15%
Middle aged man with de novo heart failure. Diagnosed with dilated cardiomyopathy with severely reduced EF. The ECG shows bifascicular block and left atrial enlargement. Multi chamber enlargement and conduction blocks are common in dilated cardiomyopathy. Sinus tachycardia is a common finding with severely depressed EF. None of the other anwers are fully compatible with the ECG.
CASE #6 Clinical scenario: Asymptomatic patient with known Apical HCM
SR and large QRS voltages. Secondary repolarization abnormalities are present in the form of deep symmetric TWI in multiple leads which is typical of ApHCM.
CASE #7 clinical scenario: Baseline (old) ECG of patient who suffered V-fib arrest during sleep (press for ECG)
Type I Brugada morphology. This patient experienced V-fib arrest while sleeping. Brugada syndrome (BRS) and Early Repolarization Syndrome (ERS) constitute the J wave syndromes (JWS). JWS are clinically similar in their presentation. CA usually occurs during bradycardia and in situations characterized by increased vagal tone as occurs during sleep. Genetic testing revealed SCN5A mutation linked to BrS.
CASE #8 clinical scenario: Baseline ECG of an African American male
This ECG pattern may be confusing if you have not seen it before. If you have, it is instantly recognizable as benign T wave inversion (BTWI). Markedly increased voltage, distinct J waves with upward sloping STE and TWI in leads with STE. This ECG pattern is more commonly found in males of African heritage.
CASE #9 clinical scenario: Chest pain and RCA occlusion at cath
Very subtle STE and (possible) hyperacute T waves inferior leads. What makes this ECG diagnostic of OMI is the reciprocal change in aVL and ST flattening in V2-V3 that indicates associated posterior OMI. The patient was found to have a 100% occlusion of the pRCA.
CASE #10 clinical scenario: Obtunded, shocky with LMCA OMI at cath
ECG obtained from a 70 yo ill-appearing male. ECG shows afib with RBBB and LAFB. There is ST-segment elevation in leads V4-V6, I and aVL with several leads showing extensive ST depression. This patient arrested and received thrombolytics. He survived transport to the cath lab where LM was stented. LM is the best answer among the choices given. There is no "single" ECG picture for LM occlusion.